Contents
- 1 Pregnancy: Preeclampsia vs. Eclampsia
- 1.0.1 What are preeclampsia and eclampsia?
- 1.0.2 What causes preeclampsia and eclampsia?
- 1.0.3 Who is at risk for preeclampsia and eclampsia?
- 1.0.4 What are the symptoms of preeclampsia and eclampsia?
- 1.0.5 How are preeclampsia and eclampsia diagnosed?
- 1.0.6 What is the treatment for preeclampsia and eclampsia?
- 1.0.7 What are complications of preeclampsia and eclampsia?
- 1.0.8 Can preeclampsia and eclampsia be prevented?
- 1.0.9 What is the outlook for preeclampsia and eclampsia?
- 1.0.10 Subscribe to MedicineNet’s Pregnancy & Newborns Newsletter
Pregnancy: Preeclampsia vs. Eclampsia
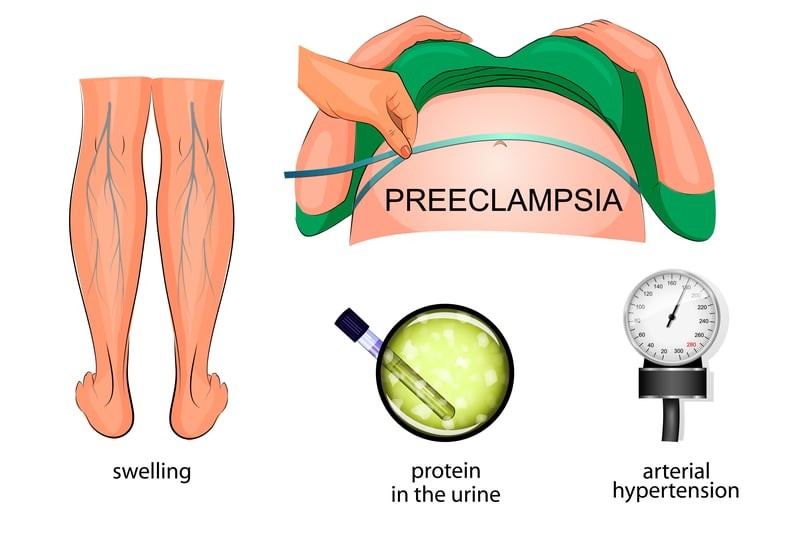
Preeclampsia and eclampsia are characterized by high blood pressure, protein in the urine, and swelling of the feet, legs, and hands.
- Preeclampsia is hypertension and proteinuria during pregnancy.
- Preeclampsia typically occurs after the 34th week of pregnancy, but it can develop after delivery.
- Preeclampsia and eclampsia commonly occur during a woman’s first pregnancy, with increased risk for pregnant teens and women over 40.
- Eclampsia is seizures in a woman with severe preeclampsia, causing a 2% mortality rate.
- Delivery of the baby is the only cure for preeclampsia.
- Mild preeclampsia can be managed with close monitoring, corticosteroids for lung development, magnesium sulfate for seizure prevention, and sometimes blood pressure medications.
- Preeclampsia can result in preterm delivery, low amniotic fluid, and sub-optimal fetal growth.
- Maternal complications include liver and kidney failure, bleeding and clotting disorders, and HELLP syndrome.
- Swelling of the feet, legs, and hands can occur in normal pregnancy and may not be related to preeclampsia.
- Eclampsia is preeclampsia with seizures.
- Preeclampsia cannot be prevented.
- The cause of preeclampsia and eclampsia is not fully understood, but it involves vascular and placental abnormalities, genetic factors, and potential immune system issues.
What are preeclampsia and eclampsia?
Preeclampsia is hypertension and proteinuria during pregnancy that can progress to eclampsia, which is seizures in a woman with preeclampsia. Eclampsia is a serious condition that can be fatal. Approximately 1 in 200 cases of preeclampsia progress to eclampsia. Preeclampsia affects 2% to 7% of healthy women who have never given birth.
Preeclampsia usually occurs after the 20th week of pregnancy and can continue for several weeks after delivery. It is more common after the 34th week of gestation and can occur postpartum within 48 hours. First-time pregnancies, pregnant teens, and women over 40 have an increased risk of preeclampsia and eclampsia.
What causes preeclampsia and eclampsia?
The exact cause is not fully understood, but it is believed to involve vascular and placental abnormalities, genetic factors, and potentially the immune system. Nutritional factors, obesity, and certain diseases may also contribute. Research suggests problems in the immune response of women with preeclampsia.
Who is at risk for preeclampsia and eclampsia?
Risk factors for preeclampsia and eclampsia include age (teens or women over 40), previous preeclampsia/eclampsia, obesity, pre-existing high blood pressure, pregnancy through egg donation or donor insemination, family history, certain diseases, multiple gestation, and sickle cell disease.
IMAGES
What are the symptoms of preeclampsia and eclampsia?
Most women with mild preeclampsia do not have symptoms, but they may have proteinuria and elevated blood pressure. Swelling of the feet, legs, and hands can occur, but it is not necessarily related to preeclampsia. Sudden weight gain over 1 to 2 days may also be a symptom.
Severe preeclampsia can cause dizziness, headaches, nausea, vomiting, abdominal pain, vision changes, reflex changes, altered mental state, fluid in the lungs, and decreased urine output. Eclampsia is preeclampsia with seizures that are typically preceded by headache and vision disturbances. Severe preeclampsia may also result in low platelet count.
Most symptoms of preeclampsia go away within 1 to 6 weeks after delivery.
How are preeclampsia and eclampsia diagnosed?
Preeclampsia is diagnosed through urinalysis to check for proteinuria and blood pressure measurements. Blood tests and other monitoring may also be done. Research suggests that Congo red spotting tests may be more accurate indicators of preeclampsia than standard urine dipstick tests.
There are no predictive tests for preeclampsia.
What is the treatment for preeclampsia and eclampsia?
The only cure is delivery of the baby. The decision on when to induce labor or perform a cesarean section depends on the severity of the condition, gestational age, and fetal health. Mild preeclampsia can be managed with monitoring, steroid drugs for lung maturity, magnesium sulfate for seizure prevention, and blood pressure medications if necessary.
Severe preeclampsia may require delivery after 34 weeks of gestation, with magnesium sulfate and blood pressure medications administered. Eclampsia is a medical emergency and is treated with medications to control seizures and stabilize blood pressure.
What are complications of preeclampsia and eclampsia?
Preeclampsia can lead to restricted blood flow to the placenta and the fetus, resulting in delayed growth, low birth weight, preterm delivery, and oligohydramnios. Placental abruption can occur, causing life-threatening bleeding and fetal death. Severe preeclampsia can affect liver and kidney function, leading to HELLP syndrome and potential stroke.
Can preeclampsia and eclampsia be prevented?
There is currently no known way to prevent these conditions. Prompt recognition and management are important for better outcomes, so routine health screenings during pregnancy are recommended.
What is the outlook for preeclampsia and eclampsia?
Most women with mild preeclampsia have good pregnancy outcomes. Eclampsia has a 2% mortality rate. The recurrence risk for preeclampsia varies depending on the onset and severity of the condition. Women with early onset and severe preeclampsia have the highest recurrence risk. Women with mild preeclampsia have a lower risk of recurrence. Preeclampsia may also increase the risk of cardiovascular disease later in life, particularly for women with early onset of severe preeclampsia.
Subscribe to MedicineNet’s Pregnancy & Newborns Newsletter
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and I understand that I may opt out of MedicineNet subscriptions at any time.
Medically reviewed by Wayne Blocker, MD; Board Certified Obstetrics and Gynecology