Contents
- 1 Leptospirosis
- 1.0.1 What causes leptospirosis?
- 1.0.2 Is leptospirosis contagious? What is the contagious period?
- 1.0.3 What is the incubation period?
- 1.0.4 What are risk factors?
- 1.0.5 What are leptospirosis symptoms and signs?
- 1.0.6 What specialists treat leptospirosis?
- 1.0.7 How do physicians diagnose leptospirosis?
- 1.0.8 What is the treatment for leptospirosis?
- 1.0.9 What is the prognosis of leptospirosis?
- 1.0.10 Is a vaccine available for leptospirosis?
Leptospirosis
Leptospirosis is a disease caused by bacteria (Leptospira interrogans) that produce a wide range of symptoms that may occur in two phases; some patients may develop kidney or liver failure, respiratory failure, meningitis, or even death. The bacterial infection is spread by the urine of infected animals from many species, both domesticated (such as dogs and horses) and wild infected animals (such as rodents or wild pigs). It is a zoonotic disease because it occurs in wild animals. The bacteria can survive in freshwater and soil for months. The disease is most common in temperate and tropical climates. The infecting bacteria occur worldwide (for example, in the United States, Leptospira has been found in Hawaii’s freshwater ponds and waterfalls).
What causes leptospirosis?
The cause of leptospirosis is bacteria (genus Leptospira and species interrogans), a Gram-negative spirochete. The Leptospira bacteria infect many types of animals (many wild animals, rodents, dogs, cats, pigs, horses, cattle, for example) that subsequently contaminate water, lakes, rivers, soil, and crops when they urinate. The bacteria then infect humans through breaks in the skin or mucus membranes or when people ingest them. The bacteria multiply in the liver, kidneys, and central nervous system. Person-to-person transfer of this disease is rare.
Is leptospirosis contagious? What is the contagious period?
Leptospirosis is weakly contagious. Humans can shed leptospirosis in the urine during and after illness, and individuals exposed to the urine of infected humans may become infected. For example, although the bacteria are not airborne and have a low risk of being in saliva, individuals handling wet bedding or blood-soaked material from an infected person can increase the chances of getting the infection. There are a few reports of transmission between sexual partners, but the incidence of this type of spread seems very low. Unfortunately, pregnant mothers who get leptospirosis can infect their fetus.
The contagious period depends on how long viable organisms are shed in the urine. Most individuals will shed organisms in the urine for a few weeks, but there are reports that humans can continue to shed the organisms in urine for as long as 11 months. Some experts suggest that there is a risk for up to 12 months after getting the initial infection.
IMAGES
What is the incubation period?
The incubation period for leptospirosis is approximately seven to 12 days but may range from two to 30 days.
What are risk factors?
Risk factors include occupational exposure to farm animals, wild animals, and contaminated water and soil (farmers, slaughterhouse workers, veterinarians, miners, military personnel, disaster workers, and victims, for example). People who participate in outdoor activities such as camping or kayaking are also at higher risk for infection. Any exposure to sewage or animal waste, including stools from infected dogs, increases the risk of getting leptospirosis. Heavy rainfall may cause the bacterial infection to increase in a population that experiences flooding. This is evidenced by reported deaths from leptospirosis due to flooding in Puerto Rico.
What are leptospirosis symptoms and signs?
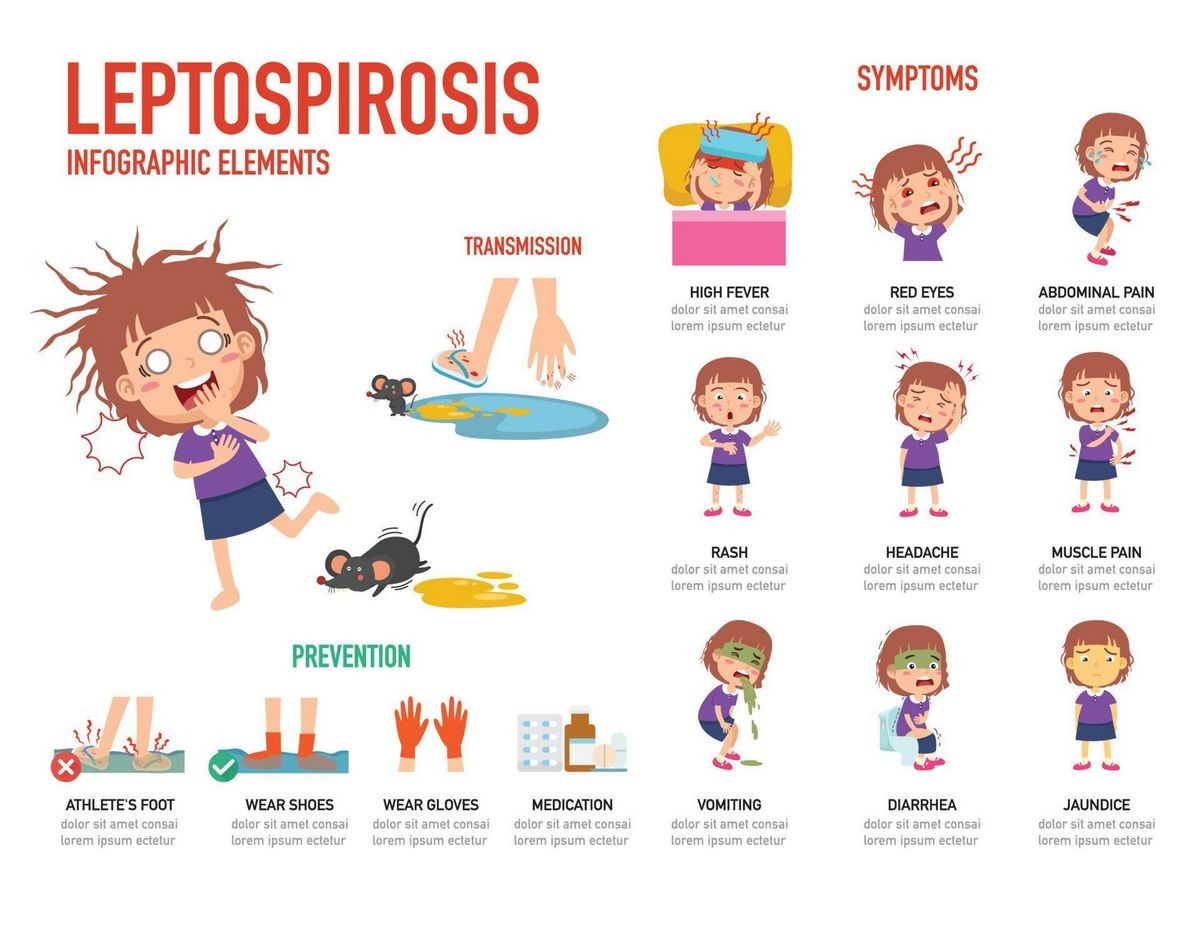
The symptoms and signs of leptospirosis are variable and similar to those seen in many other diseases (dengue fever, hantavirus, brucellosis, malaria, and others). Symptoms can arise about two days to four weeks after exposure to the bacteria. Some people have no symptoms, while others may exhibit:
- High fever
- Chills
- Headache
- Muscle aches and pain
- Fatigue
- Sore throat
- Abdominal pain
- Vomiting
- Diarrhea
- Jaundice
- Pain in the joints or muscles
- Rash
- Reddish eyes
These symptoms usually occur in the first phase of the infection, and when present, they often occur abruptly. Some patients resolve their symptoms and do not progress to the second phase. Others may briefly recover but relapse (about 5%-10%) with more severe symptoms and organ damage in the severe form of the disease. The second-phase symptoms may overlap with the first-phase symptoms in severe disease and include jaundice, renal failure, pulmonary hemorrhage, cardiac arrhythmias, pneumonitis, and septic shock. This is the second phase of leptospirosis, called Weil’s disease. If it’s not treated, it may not resolve for several months, and some patients may develop long-term complications such as kidney and lung problems. The death rate is about 1%-5%.
What specialists treat leptospirosis?
Clinic doctors, primary care doctors, pediatricians, and emergency medicine specialists often treat leptospirosis in countries where it is endemic and the patients are in the first phase of the disease. Other specialists are often consulted if the patient begins to enter the second phase of the disease, including critical care, infectious-disease, hospitalists, internists, pulmonologists, cardiologists, and kidney specialists.
How do physicians diagnose leptospirosis?
Physicians make a presumptive diagnosis based on the patient’s history and physical exam. Only specialized labs perform serological tests for leptospirosis serogroups (specific types of the bacteria that react with certain antibodies). Health care professionals may perform definitive tests by isolating the bacteria from the patient (blood or CSF) or by a positive microscopic agglutination test. Other tests may provide additional evidence of infection. Patients with severe symptoms should be treated as confirmatory tests are time-consuming.
What is the treatment for leptospirosis?
Although there is controversy about using antibiotics in the first phase of leptospirosis, antibiotics are recommended for treatment of patients with phase two or more severe symptoms. Some patients may require IV antibiotics and supportive hospital care such as rehydration. For those who choose to treat phase-one patients, antibiotics are used, and many choose to treat with doxycycline.
What is the prognosis of leptospirosis?
Overall, the prognosis of leptospirosis is good. Many people become infected and spontaneously recover without treatment. However, the prognosis worsens as the symptoms increase. People with Weil’s disease may have a prognosis ranging from good to poor, depending on their response to treatment. Pregnant women who become infected have a high rate of fetal mortality, especially if they acquire the disease early in pregnancy.
Is a vaccine available for leptospirosis?
A leptospirosis vaccine is not currently available in the U.S.; however, high-risk workers in some European and Asian countries may have access to a vaccine. Unfortunately, the vaccines are serovar-specific and thus do not offer widespread protection as there are over 200 serovars. Some vaccines are available for animals but these, like the human vaccines, are only effective against a narrow range of serovars. In addition, side effects of the vaccine can cause painful swelling. Chemoprophylaxis (using drugs to prevent illness) is possible under certain circumstances. Some individuals who may have high short-time risk may take doxycycline, beginning one to two days before potential exposure to have about a 95% chance of preventing infection with chemoprophylaxis. This preventive treatment is not recommended for long-term exposure. Avoiding contact with animal excrement, good hygiene, and avoiding contaminated water and soil are other ways to reduce the chance of getting leptospirosis. Dogs, and many other animals, can be infected with leptospirosis. Veterinarians have access to vaccines that can protect (or prevent) leptospirosis in dogs and other animals for at least 12 months. This vaccination may help protect the animals’ owners and other local or family-owned animals from the disease for approximately one year.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
Brett-Major, D.M., and R. Coldren. "Antibiotics for Leptospirosis." Cochrane Database Syst Rev 2 Feb. 15, 2012.
Brett-Major, D.M., and R. Coldren. "Antibiotics for Leptospirosis." Cochrane Database Syst Rev 2 Feb. 15, 2012.


