Contents
Can No Activity Cause Dizziness?
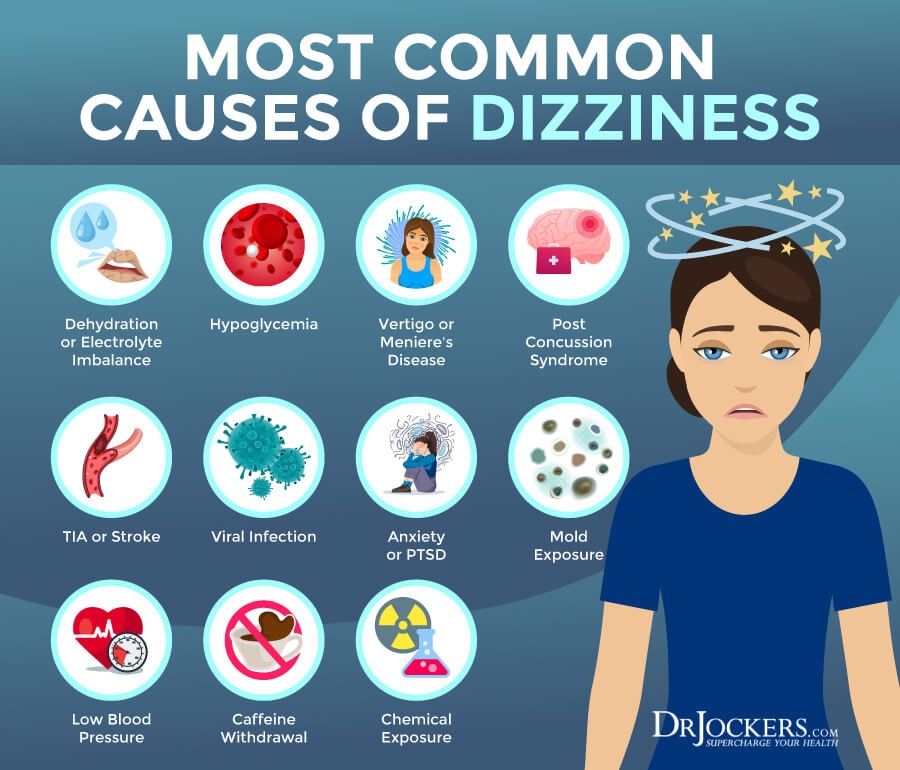
Physical inactivity and low fitness levels have been identified as risk factors for various metabolic and circulatory changes that cause symptoms, including dizziness, especially in older individuals.
Osteoporosis and muscle weakness due to inactivity contribute to dizziness from weakening cervical muscles and bones.
- Dizziness is a common symptom in the elderly, which is critical because it increases the risk of falls, a major factor in morbidity and mortality among older individuals.
- Inactivity can cause orthostatic hypotension or low blood pressure when changing body position, leading to dizziness in inactive people. This is due to compromised blood vessels that become engorged, reducing circulation to the brain.
- Muscles contract and relax to pump blood back from the extremities. When activity levels are low or muscles weaken, this process is impaired.
- Reduced activity limits proper chest expansion needed for improved lung function during increased activity.
Physical inactivity is a significant risk factor for age-related disorders. A sedentary lifestyle can accelerate the aging process. Promoting regular exercise and a healthy lifestyle can have potential anti-aging effects.
16 Symptoms of Orthostatic Hypotension
Orthostatic hypotension occurs when there is a significant reduction in blood pressure upon standing from a seated or supine position.
Orthostatic hypotension, also known as postural hypotension, is caused by changes in posture, such as transitioning from sitting to standing.
In most cases, this condition is asymptomatic, but some individuals may experience the following symptoms:
- Dizziness
- Lightheadedness
- Blurred vision
- Fatigue
- Nausea
- Palpitations
- Headache
- Brain fog
- Confusion
- Excessive sweating above the level of injury
- Muscle weakness
- Syncope
- Dyspnea
- Chest pain
- Neck and shoulder pain
- Unexplained falls
Orthostatic hypotension is a common disorder, affecting approximately 10 to 30 percent of the elderly population.
8 Common Causes of Orthostatic Hypotension
When sitting or lying down, blood tends to pool in the veins of the legs. Standing causes a drop in systemic blood pressure as less blood returns to the heart against gravity.
Normally, sensors in the aorta and carotid arteries detect this blood pressure decrease and adjust the caliber of peripheral blood vessels to maintain normal blood pressure. When this process fails, orthostatic hypotension occurs.
Orthostatic hypotension can be caused by multiple factors, including:
- Dehydration: Insufficient fluid intake increases the risk of orthostatic hypotension. Causes may include fever, vomiting, diarrhea, excessive sweating, excessive alcohol consumption, or constant exposure to a hot environment.
- Cardiac problems: Certain heart conditions impair the body’s ability to maintain blood pressure, such as low heart rate, structural or functional valve problems, or heart failure.
- Endocrine problems: Conditions affecting blood pressure regulation, such as thyroid issues, adrenal insufficiency, or high/low blood glucose levels, can cause orthostatic hypotension.
- Neurodegenerative disorders: Underlying nervous system disorders, like Parkinson’s disease, multiple system atrophy, Lewy body dementia, or amyloidosis, increase the risk of orthostatic hypotension.
- Aging: Orthostatic hypotension is associated with prolonged standing, chronic medical conditions, and becomes more common with age and frailty. Increased blood flow during digestion can cause blood pressure to drop.
- Medication: Drugs used for high blood pressure, anxiety, depression, and erectile dysfunction can cause orthostatic hypotension, such as beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, nitrates, angiotensin II blockers, diuretics, and prostate medications.
- Prolonged bed rest: Extended bed rest can lead to impaired blood pressure regulation during movement and postural changes, resulting in orthostatic hypotension.
- Pregnancy: In pregnancy, rapid uterine enlargement places pressure on the abdominal aorta, contributing to orthostatic hypotension.
Orthostatic hypotension can be exacerbated by certain conditions, such as anemia and spinal cord problems (syringomyelia). Spinal cord diseases can cause orthostatic hypotension through changes in sympathetic activity, impaired baroreflex, and salt and water imbalance.
Treatment Options for Orthostatic Hypotension
The goal of treating orthostatic hypotension is to restore normal blood pressure. This typically involves increasing blood volume, reducing blood pooling, and aiding blood flow throughout the body.
Treatment often targets the underlying cause, such as addressing dehydration or heart failure rather than low blood pressure alone.
One of the simplest treatments for moderate orthostatic hypotension includes:
- Hydration
- Quickly sitting or lying down when feeling lightheaded upon standing
- Adjusting medication dosage or discontinuing medications contributing to low blood pressure
Other treatment options for orthostatic hypotension may include:
- Lifestyle changes: Doctors may recommend lifestyle modifications such as drinking plenty of fluids, avoiding alcohol and overheated environments, elevating the head of the bed, sitting with legs uncrossed, standing up slowly, taking breaks before walking, increasing salt intake (if no high blood pressure), and consuming small, low-carbohydrate meals after meals decrease blood pressure.
- Wearing compression stockings, garments, or abdominal binders to prevent blood pooling in the legs and alleviate symptoms of orthostatic hypotension.
- Prescription medication options:
- Alpha-adrenergic agonists
- Mineral corticoids
- Nonselective alpha-and beta-receptor agonists
- Combination therapies
Drug side effects will be monitored, and dosages will be adjusted accordingly.
Exercise has been shown to increase bone density and reduce the risk of dizziness, lightheadedness, and falls in individuals of all ages.
However, inactivity decreases overall bone calcium and can lead to various neurological and orthopedic complications. Staying active is crucial for maintaining good health, even as one ages.