Contents
Beta Blockers vs. ARBs
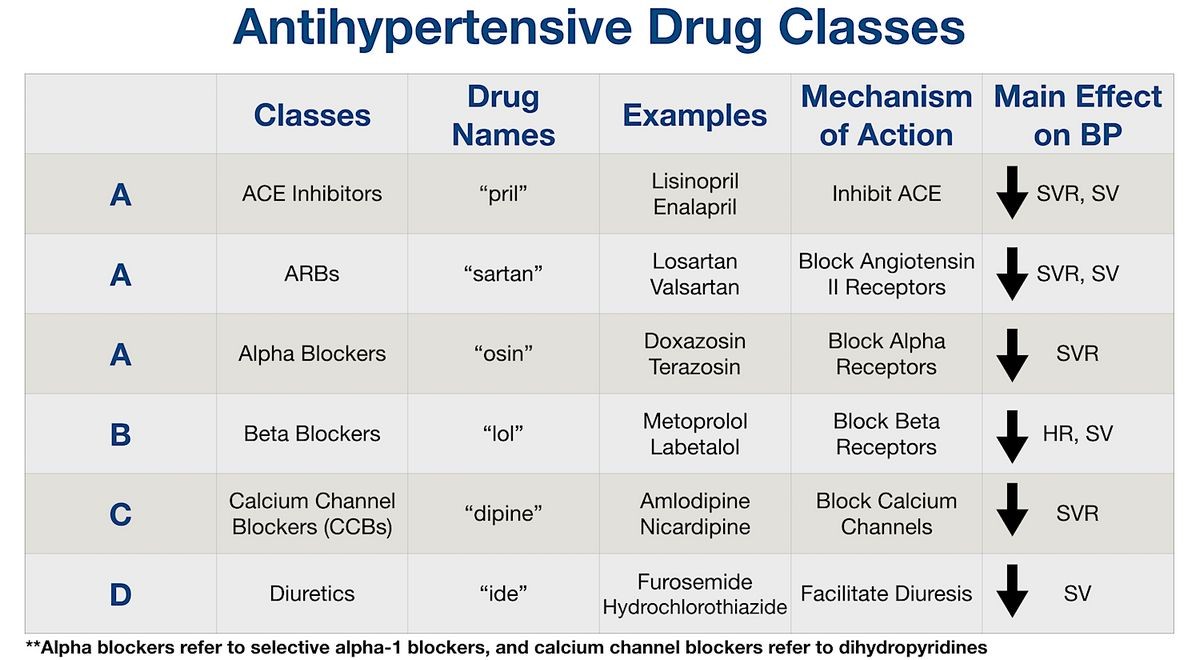
Beta blockers, or beta-adrenergic blocking agents, block norepinephrine and epinephrine from binding to beta-receptors on nerves. This dilates blood vessels, reducing heart rate and blood pressure.
- Beta blockers treat high blood pressure, angina, heart failure, abnormal heart rhythms, tremors, pheochromocytoma, migraine prevention, hypertrophic subaortic stenosis, hyperthyroidism, panic disorder, anxiety, akathisia, eye pressure from glaucoma, and aggressive behavior.
- Beta blockers also prevent future heart attacks and death after a heart attack.
Angiotensin II receptor blockers (ARBs) block the action of angiotensin II, preventing it from binding to receptors on blood vessel muscles. This causes blood vessels to dilate and reduces blood pressure, making it easier for the heart to pump blood.
- When angiotensin II can’t bind to receptors, blood vessels enlarge and blood pressure decreases.
- ARBs treat high blood pressure, heart failure, prevent kidney failure in people with diabetes or high blood pressure, prevent diabetes in patients with high blood pressure and an enlarged heart, and reduce the risk of stroke.
- ARBs may also prevent atrial fibrillation from recurring.
Side Effects of Beta Blockers vs. ARBs
Beta blocker side effects
Beta blockers may cause:
Other important side effects include:
As an extension of their beneficial effect, beta blockers slow heart rate and reduce blood pressure. However, they may cause adverse effects such as heart failure or heart block in patients with heart problems.
Beta blockers should not be withdrawn suddenly, as it may worsen angina and cause heart attacks, abnormal heart rhythms, or sudden death.
Central nervous system effects of beta blockers include:
Beta blockers that block β2 receptors may cause shortness of breath in asthmatics.
Sexual dysfunction may occur, as with other drugs used for treating high blood pressure.
Beta blockers may cause low or high blood glucose and mask symptoms of low blood glucose in people with diabetes. Other serious side effects include:
- Raynaud’s phenomenon
- Lupus erythematosus
- Bronchospasm
- Serious allergic reactions
- Erythema multiform
- Steven Johnson Syndrome
- Toxic epidermal necrolysis
ARB side effects
ARBs are well tolerated. The most common side effects are:
- Cough
- Elevated potassium levels in the blood (hyperkalemia)
- Low blood pressure
- Dizziness
- Headache
- Drowsiness
- Diarrhea
- Abnormal taste sensation (metallic or salty taste)
- Rash
- Orthostatic hypotension (low blood pressure upon standing)
- Fatigue
- Indigestion
- Upper respiratory tract infection
Cough occurs less often with ARBs compared to ACE inhibitors.
The most serious, but rare, side effects are:
- Kidney failure
- Liver failure (hepatitis)
- Serious allergic reactions
- Decrease in white blood cells
- Decrease in blood platelets
- Swelling of tissues (angioedema)
Rhabdomyolysis has been reported in patients receiving ARBs.
Individuals with narrowing of both arteries supplying the kidneys or severe reactions to ARBs should avoid them.
Like other antihypertensives, ARBs have been associated with sexual dysfunction.
Drug Interactions with Beta Blockers and ARBs
Beta blocker drug interactions
- Combining propranolol (Inderal) or pindolol (Visken) with thioridazine (Mellaril) or chlorpromazine (Thorazine) may result in low blood pressure and abnormal heart rhythms.
- Dangerous elevations in blood pressure may occur when clonidine (Catapres) is combined with a beta blocker, or when clonidine or beta blocker is discontinued after their concurrent use.
- Phenobarbital and similar agents may reduce blood levels of propanolol (Inderal) or metoprolol (Lopressor, Toprol XL), reducing effectiveness.
- Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) may counteract the blood pressure reducing effects of beta blockers.
- Beta blockers may prolong hypoglycemia and mask symptoms in diabetics taking insulin or other diabetic medications.
ARB drug interactions
- ARBs have few interactions with other drugs.
- ARBs may increase blood levels of potassium, so caution should be taken with potassium supplements, salt substitutes, or other drugs that increase potassium.
- ARBs may increase blood concentration of lithium and lead to increased side effects.
- Rifampin reduces blood levels of losartan, and fluconazole reduces the conversion of losartan to its active form.
- ARBs should not be combined with ACE inhibitors or aliskiren.
Types of Beta Blockers and ARBs
Beta blockers:
- acebutolol (Sectral)
- atenolol (Tenormin)
- betaxolol (Kerlone and Betoptic S)
- bisoprolol fumarate (Zebeta)
- carteolol (Cartrol, discontinued)
- carvedilol (Coreg)
- esmolol (Brevibloc)
- labetalol (Trandate, Normodyne discontinued)
- metoprolol (Lopressor, Toprol XL)
- nadolol (Corgard)
- nebivolol (Bystolic)
- penbutolol (Levatol)
- pindolol (Visken, discontinued)
- propranolol (Hemangeol, Inderal LA, Inderal XL, InnoPran XL)
- sotalol (Betapace, Sorine)
- timolol (Blocadren, discontinued)
- timolol ophthalmic solution (Timoptic, Betimol, Istalol)
ARBs include:
azilsartan (Edarbi), candesartan (Atacand), eprosartan (Teveten), irbesartan (Avapro), telmisartan (Micardis), valsartan (Diovan), losartan (Cozaar), and olmesartan (Benicar).
Summary
Beta blockers and ARBs both dilate blood vessels through different actions on the nervous system. They are used to treat high blood pressure and heart failure.


