Contents
- 1 Primary Sclerosing Cholangitis (PSC)
- 1.0.1 Causes of primary sclerosing cholangitis
- 1.0.2 Risk factors for primary sclerosing cholangitis
- 1.0.3 Signs and symptoms of primary sclerosing cholangitis
- 1.0.4 Diagnosis of primary sclerosing cholangitis
- 1.0.5 Treatment options for primary sclerosing cholangitis
- 1.0.6 Medications for primary sclerosing cholangitis
- 1.0.7 Liver transplantation
- 1.0.8 Prognosis and life expectancy
- 1.0.9 Complications of primary sclerosing cholangitis
- 1.0.10 Prevention of primary sclerosing cholangitis
Primary Sclerosing Cholangitis (PSC)
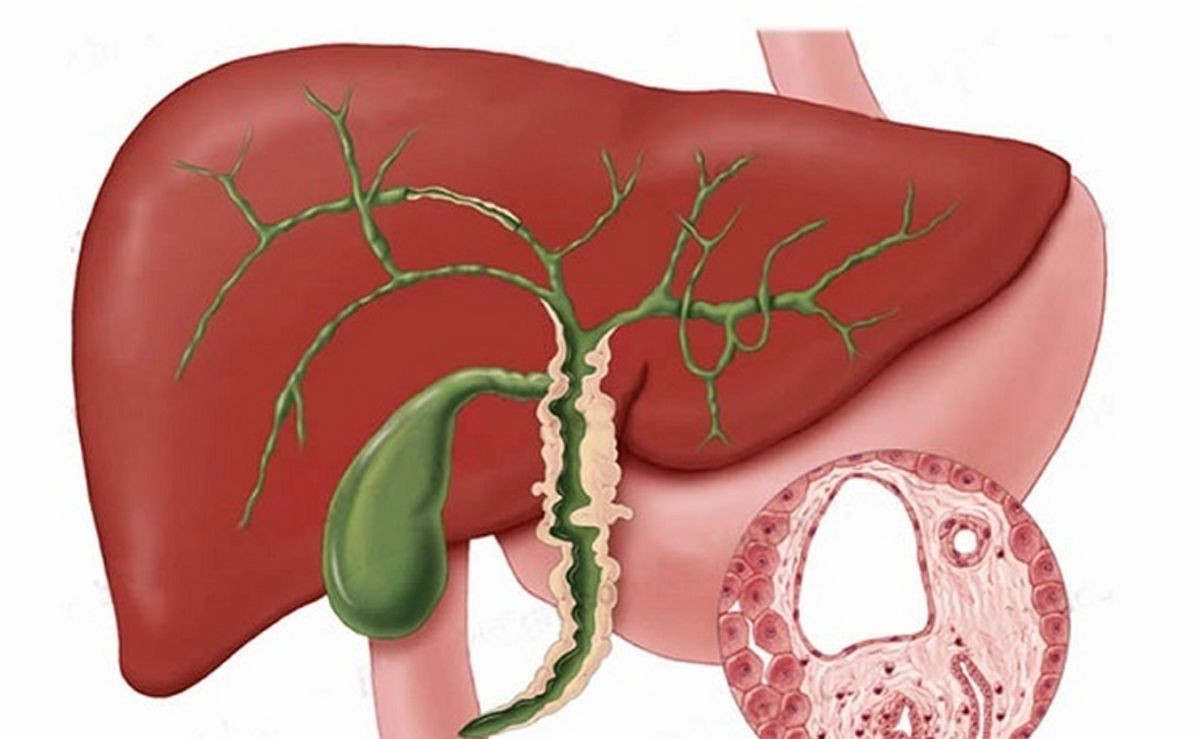
Primary sclerosing cholangitis is a disease in which the liver’s bile ducts become inflamed, narrow, and hinder proper bile flow.
The liver produces bile to aid in food digestion. Bile travels through the bile ducts in the biliary tree and enters the gallbladder. When food reaches the small intestine, bile helps break down fat into fatty acids, facilitating absorption and utilization by the body. Bile also facilitates the absorption of fat-soluble vitamins (A, D, E & K).
Inflammation and narrowing of the bile ducts impede bile flow, leading to increased pressure within the liver and inflammation of liver cells. Over time, decreased blood flow within the liver due to inflammation raises pressure in the portal vein. This results in portal hypertension, leading to swelling of the esophageal, gastric, and intestinal veins (varices) as well as splenomegaly (enlarged spleen).
The disease progresses as scar tissue replaces dead liver cells, leading to cirrhosis and liver failure.
Causes of primary sclerosing cholangitis
Although the cause of PSC is unknown, there is an association with inflammatory bowel disease, particularly ulcerative colitis. It is believed that an autoimmune component may trigger inflammation and narrowing of the bile ducts in the liver.
Risk factors for primary sclerosing cholangitis
PSC is more common in men aged 20-30 and is often associated with inflammatory bowel disease, predominantly ulcerative colitis and less commonly Crohn’s disease. In individuals without inflammatory bowel disease, PSC is more prevalent in females and older individuals.
Signs and symptoms of primary sclerosing cholangitis
In the early stages, PSC is asymptomatic. Symptoms only occur when cholestasis, the impaired drainage of bile from the liver, develops. Initial symptoms include fatigue and itching. Elevated bilirubin levels in the blood may cause jaundice or yellowing of the skin. Inflammation of the liver may result in pain below the ribs in the upper right abdomen. Bile duct obstruction can lead to sludge formation and increase the risk of infection, causing fever and increased pain.
The disease progresses with symptoms appearing intermittently over months and years. Cirrhosis can develop, leading to decreased liver function. Complications associated with cirrhosis include bleeding from varices, ascites (abdominal fluid collection), easy bruising, and confusion due to hepatic encephalopathy.
Diagnosis of primary sclerosing cholangitis
PSC may remain asymptomatic for several years. Healthcare professionals should suspect PSC in patients with inflammatory bowel disease, specifically ulcerative colitis.
Physical examination may reveal an enlarged liver, tenderness in the upper right abdomen, an enlarged spleen, jaundiced or yellow skin, and evidence of intense itching. In advanced cirrhosis, symptoms may include skin bruising, ascites, gastrointestinal bleeding, and mental confusion.
Blood tests can assess liver function and bile duct blockages. Imaging tests, such as ultrasound and magnetic resonance cholangiogram, help evaluate liver and bile duct structure. If diagnosis remains uncertain, a biopsy may be performed to analyze liver tissue under a microscope.
QUESTION
Treatment options for primary sclerosing cholangitis
Treatment for PSC focuses on monitoring disease progression and managing symptoms and complications. Liver transplantation is the only curative option for individuals with cirrhosis and impaired liver function.
ERCP (endoscopic retrograde cholangiopancreatography), balloon dilatation, and stent placement can potentially open blocked larger bile ducts. Surgery may be considered to remove scarred and blocked bile ducts and reconnect normal ones.
Medications for primary sclerosing cholangitis
No medication is approved specifically for treating PSC. However, medications can help control symptoms. Ursodiol may improve liver function but has not been proven to increase survival. Immunosuppressive medications have not proven effective. Antihistamines and bile salt-binding medications can alleviate itching. Antibiotics may be necessary to treat infections. Malnutrition caused by impaired nutrient absorption may require vitamin supplements and dietary changes.
Liver transplantation
Liver transplantation is the only curative option for PSC patients with liver failure. The three-year survival rate for liver transplants is approximately 81%, with a five-year survival rate of about 75%. PSC can potentially recur in the transplanted liver.
Prognosis and life expectancy
Aside from liver transplantation, no effective treatments exist for PSC. Studies suggest a life expectancy of 9 to 18 years without liver transplantation. In the Netherlands, researchers estimate a life expectancy longer than 21 years from the time of diagnosis. Older patients, individuals with an enlarged liver and spleen, and those with persistent jaundice and elevated bilirubin levels have a poorer prognosis.
Complications of primary sclerosing cholangitis
PSC is a progressive disease that damages bile ducts, reduces bile flow, and ultimately leads to portal hypertension, cirrhosis, and liver failure. PSC is associated with an increased risk of gallbladder cancer, hepatocellular cancer, cholangiocarcinoma, and colorectal cancer in patients with inflammatory bowel disease.
Prevention of primary sclerosing cholangitis
There are currently no known preventive measures for PSC. It is vital for individuals with inflammatory bowel disease, particularly ulcerative colitis, and their healthcare professionals to be aware of the potential association with PSC and monitor for suggestive symptoms. However, PSC is only seen in 3% of inflammatory bowel disease patients.
Medical review by Venkatachala Mohan, MD, American Board of Internal Medicine with subspecialty in Gastroenterology.
Sources:
Boonstra, K., et al. "Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis." Hepatology 2013 Dec; 58(6):2045-55.
Razumilava N. et al. "Cancer surveillance in patients with primary sclerosing cholangitis." Hepatology 2011 Nov; 54(5):1842-52.


