Contents
Portal Hypertension
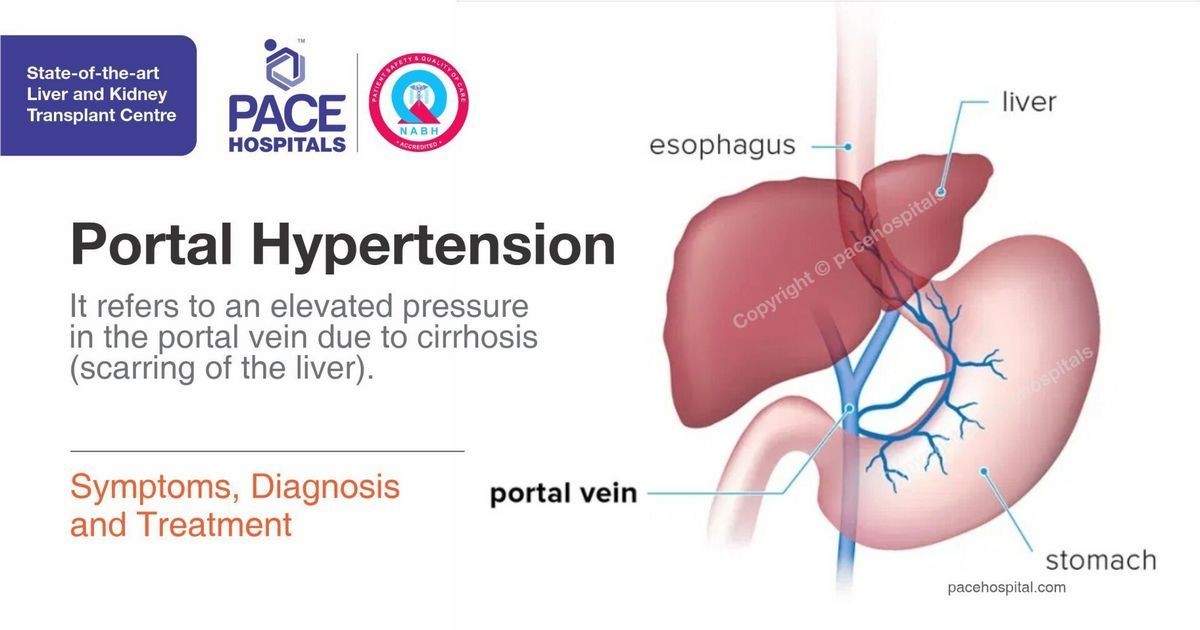
The liver serves many purposes within the body from making carbohydrates, proteins, and fats to synthesizing bile to help digest food. Because of this, the liver requires a significant blood supply. The majority of this blood supply (75%) comes from the venous system through the portal system. Blood vessels from the stomach, small intestine, pancreas, and spleen converge to form the portal vein delivering nutrients and chemical building blocks to the liver. The portal vein and hepatic artery come together to form sinusoids in the liver, spaces where the blood is filtered. From there, blood makes its way to the vena cava, the largest vein in the body returning blood to the heart.
Portal hypertension describes elevated pressure within the portal system, including the portal vein and the tributary veins that drain into it. The pressure within the portal system is not normally measured and is not an issue unless an illness or disease occurs that makes it difficult for blood to flow through the liver tissue. This damming effect increases pressure within the portal venous system and causes potential problems with liver function. Symptoms associated with liver disease might indicate the presence of portal hypertension.
Causes of Portal Hypertension
Portal hypertension occurs when there is an obstruction of blood flow through the liver, resulting in elevated pressure within the portal vein. This obstruction can be intrahepatic, pre-hepatic, or post-hepatic.
Intrahepatic Causes
Intrahepatic causes of portal hypertension include cirrhosis and hepatic fibrosis or scarring. Examples of illnesses that can cause portal hypertension include alcohol abuse, hepatitis B and C infections, fatty liver (NASH, non-alcoholic steatohepatitis), Wilson’s disease, hemochromatosis (iron overload), cystic fibrosis, primary sclerosing cholangitis, biliary atresia, and parasite infections such as schistosomiasis.
Pre-hepatic Causes
Pre-hepatic causes of portal hypertension include portal vein thrombosis or blood clots within the portal vein and congenital portal vein atresia.
Post-hepatic Causes
Post-hepatic causes are due to obstruction of blood flow from the liver to the heart and can include hepatic vein thrombosis, inferior vena cava thrombosis, and restrictive pericarditis caused by conditions like tuberculosis, fungal infections, tumors, connective tissue disorders (e.g., scleroderma), and complications from radiation therapy.
Symptoms of Portal Hypertension
Portal hypertension can lead to bypassing of the portal system, causing blood to flow through the systemic venous system to return to the heart. Symptoms are due to decreased blood flow through the liver and increased pressure within the veins where blood is shunted.
- Varices: Enlarged veins that occur in the esophagus, stomach, around the umbilicus, and in the anus and rectum.
- Esophageal and gastric varices: At risk of life-threatening bleeding and can cause vomiting blood and melena, a black, tarry stool.
- Ascites: Abnormal fluid collection within the peritoneum due to increased pressure in the portal system and decreased protein in the body.
- Hepatic encephalopathy: Causes confusion and lethargy due to the buildup of waste products and the liver’s inability to adequately filter them.
- Splenomegaly: Enlargement of the spleen due to blood backup in the portal system, leading to anemia and low platelet count.
- Decreased white blood cell counts: Increases the risk of infection, including spontaneous bacterial peritonitis.
Diagnosis of Portal Hypertension
Portal hypertension is usually diagnosed after a complication occurs. Healthcare professionals look for potential causes, including portal hypertension, when ascites or gastrointestinal bleeding develops. Diagnosis can be confirmed through specific procedures and tests, although measuring pressures within the portal vein is not routine except in certain situations.
Treatment of Portal Hypertension
Treatment for portal hypertension focuses on preventing complications, treating the underlying cause, and avoiding alcohol and certain medications. Dietary restrictions include limiting salt and protein intake. Medications like beta-blockers, nitroglycerin, and lactulose may be prescribed. Endoscopy may be required to manage esophageal and gastric varices. In some cases, a TIPS procedure may be performed to decrease pressure within the portal system. Liver transplantation may be necessary for severe cases.
Complications of Portal Hypertension
The complications of portal hypertension are associated with liver failure, including gastrointestinal bleeding, ascites, hepatic encephalopathy, and splenomegaly.
Prevention and Prognosis
The prevention of portal hypertension depends on the underlying cause, with some liver diseases being preventable. The prognosis varies depending on the extent of liver dysfunction and the patient’s compliance with treatment and lifestyle changes.
Quarrie R, et al. "Portal vein thrombosis: What surgeons need to know." International Journal of Critical Illness & Injury Science. 2018 Jun 18;8(2):73-77.
Sauerbruch T, et al. "Managing portal hypertension in patients with liver cirrhosis." F1000Research. 2018 May 2;7:F1000FacultyRev-533.


