Contents
- 1 Periodic Paralysis Syndrome
- 1.0.1 What is periodic paralysis syndrome?
- 1.0.2 Is it a genetic disease? How is it acquired?
- 1.0.3 What are the signs and symptoms?
- 1.0.4 What are the types?
- 1.0.5 What determines the type of periodic paralysis syndrome?
- 1.0.6 How is the syndrome diagnosed?
- 1.0.7 Are other diseases ruled out?
- 1.0.8 Can symptoms be managed through diet?
- 1.0.9 Subscribe to MedicineNet’s Children’s Health & Parenting Newsletter
- 1.0.10 What is the treatment?
- 1.0.11 Can the syndrome be passed on to children?
- 1.0.12 Who should consider genetic testing?
- 1.0.13 From
Periodic Paralysis Syndrome
Our doctors provide information about periodic paralysis syndrome, its types, and symptoms.
What is periodic paralysis syndrome?
Periodic paralysis syndrome causes temporary episodes of muscle weakness or paralysis. There are several types of this rare muscle disease, though the number of types is debated among doctors.
Is it a genetic disease? How is it acquired?
Most types of periodic paralysis syndrome are genetic and inherited (autosomal dominant), while others result from sporadic genetic mutations. These genetic changes result in abnormal muscle responses to various stimuli like cold environments or exercise, as well as elevated levels of electrolytes like potassium (hypokalemia). The disease can be inherited from a parent or occur due to a spontaneous mutation.
What are the signs and symptoms?
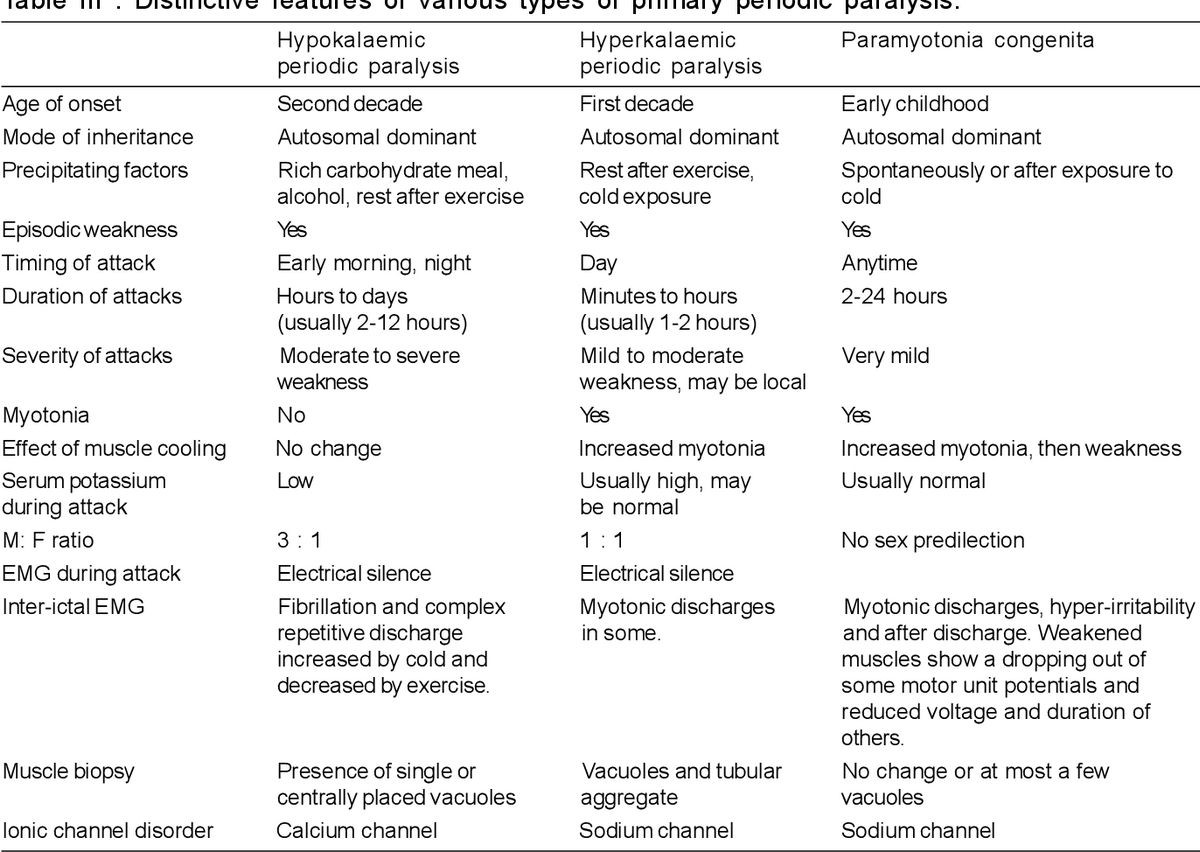
Periodic paralysis syndromes are characterized by episodes of muscle weakness that resolve over time. The duration of these episodes varies depending on the type, ranging from a few minutes to several days. Some types may lead to permanent weakness. The signs, symptoms, and causes differ for each type.
What are the types?
There are several types of periodic paralysis syndromes, including:
- Hyperkalemic periodic paralysis or hyperPP: Primarily affects children under 10 years old. Symptoms may include lagging upper eyelids, stiffness or heaviness in the muscles, and weakness that spreads to the arms and neck.
- Hypokalemia periodic paralysis 1 or hypoPP1L: Typically begins in childhood and may continue into a person’s 30s. Symptoms are due to calcium channel mutations and may include irregular heartbeats.
- Hypokalemia periodic paralysis 2 or hypoPP2: Similar to hypoPP1, but caused by sodium channel mutations.
- Normokalemic periodic paralysis: A variant of hyperPP where weakness occurs with normal variations in potassium levels.
- Thyrotoxic periodic paralysis or TPP: Affects adults in their 20s, 30s, and 40s, particularly Asian males. Weakness may involve respiratory muscles and can be triggered by hyperinsulinemia and carbohydrate intake.
- Paramyotonia congenita or PCM: Usually occurs alongside hyperPP and causes muscle stiffness, weakness in response to cold temperatures or increased activity. Caused by mutations in genes that form the sodium channels in muscles.
- Potassium aggravated myotonias or PAMS: Exercise-triggered muscle stiffness associated with potassium intake.
- Andersen-Tawil syndrome or ATS: Inconsistent potassium shifts during paralysis attacks, irregular heart rhythms, and distinctive physical features.
- Familial periodic paralysis: An umbrella term encompassing hypokalemic, hyperkalemic, thyrotoxic, and Andersen-Tawil syndromes.
However, some doctors group certain types together, such as familial periodic paralysis.
What determines the type of periodic paralysis syndrome?
The type of periodic paralysis syndrome is determined by specific genetic alterations. For example, hyperPP is associated with gene SNC4A, while hypoPP1 is associated with gene CACNAIS.
How is the syndrome diagnosed?
Periodic paralysis syndromes are diagnosed based on characteristic symptoms and additional evidence, including elevated blood levels of creatinine phosphokinase and potassium, ECG tracings, electrodiagnosis, muscle cooling, exercise testing, needle electrode examination, and muscle biopsies. Proactive testing using IV solutions may also be used, but it carries potential risks and should only be performed under the supervision of a neurologist.
Are other diseases ruled out?
Preliminary tests are conducted to rule out other causes of muscle weakness, such as licorice intoxication, laxative abuse, and severe diarrhea.
Can symptoms be managed through diet?
An appropriate diet can help reduce the frequency of attacks and muscle weakness in some cases. For example, a low-carbohydrate and low-sodium diet may decrease paralysis attacks, while a glucose-containing or low-potassium carbohydrate diet may improve weakness in hyperkalemic periodic paralysis syndrome.
Subscribe to MedicineNet’s Children’s Health & Parenting Newsletter
By clicking "Submit," you agree to the MedicineNet Terms and Conditions and Privacy Policy. You will receive emails from MedicineNet and can opt out of subscriptions at any time.
What is the treatment?
Treatment depends on the specific type of periodic paralysis syndrome and may involve medications like dichlorphenamide (Keveyis), oral or IV potassium, acetazolamide, diuretics, beta blockers, amiodarone (Cordarone), and other drugs. It is important to consider dietary factors as well.
Can the syndrome be passed on to children?
If you have a periodic paralysis syndrome, there is a 50% chance of passing it on to your children.
Who should consider genetic testing?
If one of your parents has been diagnosed or if you experience similar symptoms without a definitive diagnosis, consult with a doctor about the possibility of genetic testing for periodic paralysis syndrome.