How Many Migraines a Month Is Normal?
Migraines can be classified into distinct categories based on the number of episodes:
- Acute or episodic migraine: 1-14 migraine headaches a month
- Chronic migraine: 15 or more migraine days a month, with at least 8 fitting migraine criteria
Migraines can negatively impact your quality of life and in some cases be debilitating. When migraines start interfering with daily activities or occur more than 15 times a month, seek medical help.
What are common migraine symptoms?
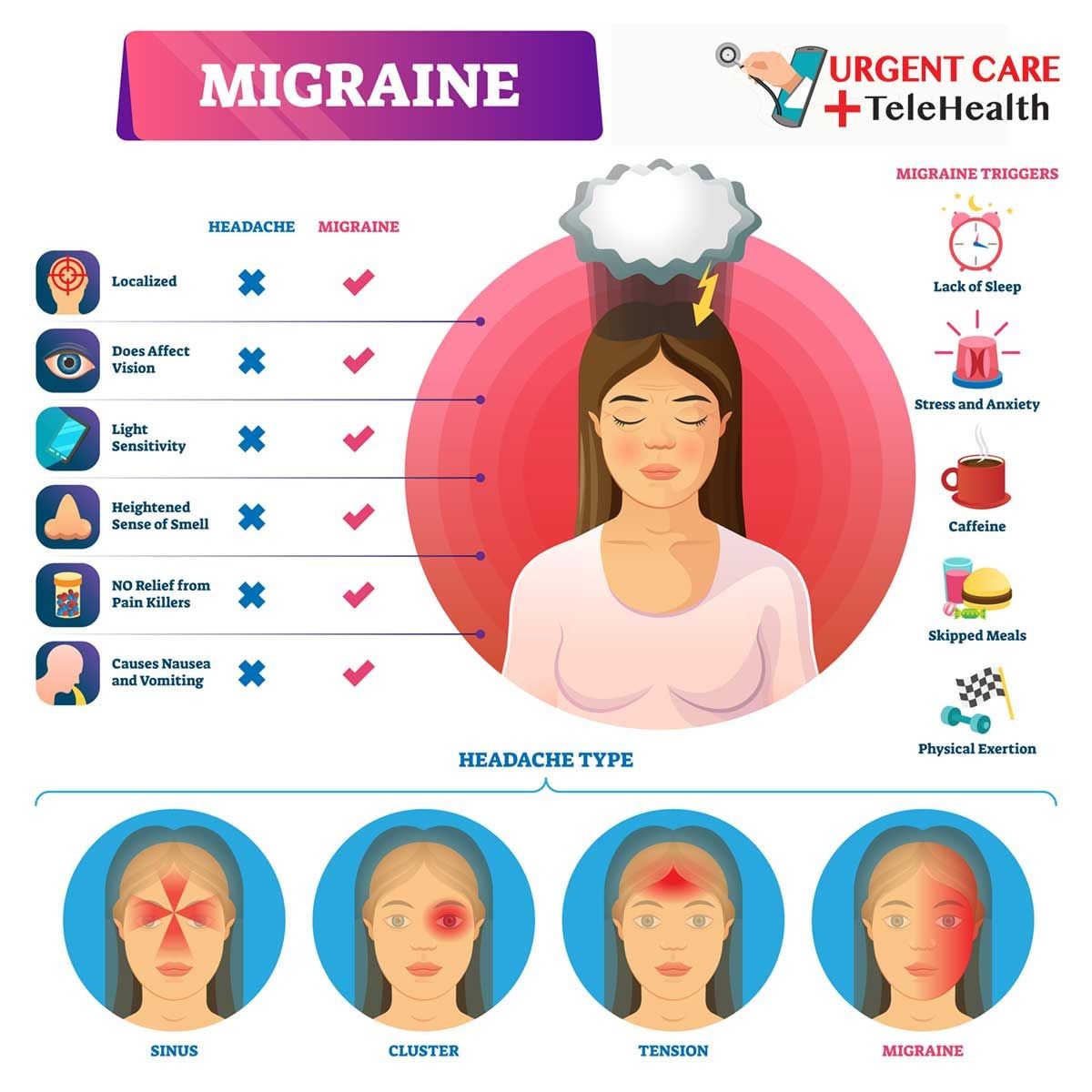
Migraines can cause a variety of symptoms and impact sufferers differently, but signs distinguish migraine episodes from tension or cluster headaches.
According to the International Headache Society, a migraine can be diagnosed with the following signs and symptoms:
At least two of the following qualities characterize the pain:
- One-sided
- Moderate to severe intensity
- Throbbing sensation
- Aggravated by movement (walking, going up stairs)
- Lasts 4-72 hours
At least one of the following associated symptoms:
- Nausea
- Vomiting
- Photophobia (sensitivity to light)
- Phonophobia (sensitivity to noise)
For some, the most distressing aspect of migraines is the pain, but the related symptoms can be equally debilitating. Related symptoms of migraine include:
- Osmophobia (sensitivity to smell)
- Aura (visual disturbances)
- Difficulty concentrating
- Problems with coordination
- Diarrhea
- Feeling extremely unwell
- Stiffness of the neck and shoulders
- Tingling, pins, and needles or numbness or even one-sided limb weakness
- Speech disturbance
- Motor weakness
- Vertigo
What are the 4 stages of migraine?
Stage 1: Prodrome
A considerable proportion of migraine sufferers get warning symptoms up to 24 hours before attacks begin, but these indicators may go unnoticed. Some symptoms include:
- Mood changes
- Nausea
- Appetite changes
- Lack of appetite
- Constipation
- Diarrhea
- Drowsiness
- Incessant yawning
- Difficulty finding the right words
- Discomfort with light and sound
- Vision problems
- Changes in behavior and being agitated and clumsy
- Muscle stiffness, particularly in the neck and shoulders
- Frequent urination
Stage 2: Aura
Aura is seen in about 20% of migraine sufferers. The most frequent aura symptoms, known as typical aura, are visual, sensory, or speech/language problems. The aura stage often lasts between 5-60 minutes. Typical disruptions include:
- Bright zigzag lines
- Flashing lights
- Blind spots
- Difficulty focusing
- Trouble speaking
- Vertigo
- Tinnitus
- Double vision
- Motor weakness
Stage 3: Headache
A migraine with aura may or may not have a gap of up to an hour between the end of the aura and the start of a headache. The headache stage may last 4 hours to 3 days.
Pain is usually throbbing and on one side of the brain, although it can affect both. Pain is also aggravated by movement.
During this period, the most common related symptoms include:
- Nausea
- Vomiting
- Sensitivity to light, sound, and smell
Stage 4: Post-drome
After a migraine attack, many people feel exhausted for 24 hours, while others may feel energized or even ecstatic.
Other common symptoms during this recovery period include weariness, nausea, and persistent sensitivity to light and sound.
What causes migraines?
The exact cause of migraines is unknown, but factors contribute to an attack. Migraines may be the result of the activation of certain areas of the brain, including the brainstem, that affect nerve signals and blood vessels.
Risk factors of migraine include:
- Family history of migraine
- Female sex (hormonal factors)
- History of anxiety and depression
- Physical, emotional, and sexual abuse
Common triggers of migraine include:
- Emotional stress
- Lack of sleep or oversleeping
- Missed, delayed, or inadequate meals
- Certain foods (chocolate, citrus, aged cheeses/meats, cultured products, and other processed foods)
- Food additives (caffeine, monosodium glutamate, aspartame, etc.)
- Alcohol
- Bright or flickering lights
- Strong smells (gasoline, perfume)
- Loud sounds
- Changes in environment, altitude, or weather
- Poor posture
- Hormonal changes (menstruation, perimenopause, or menopause)
- High impact exercises
However, each person’s triggers are unique, and migraines often result from a combination of triggers.
Episodic migraines can progress to chronic migraines over months or years, although it is unclear how episodic migraines become chronic.
Some experts believe that inflammation causes blood vessels in the brain to expand and squeeze surrounding nerves, resulting in headaches. It is conceivable that repeated bouts of inflammation make particular nerve cells in the brain more sensitive, increasing the likelihood and frequency of migraines.
Migraine Treatments:
What are your other options?
What are the best treatment options for migraine?
Effective treatments are available to reduce migraine symptoms and prevent further attacks. Treatment can be administered beforehand to prevent the number and intensity of attacks or during an attack to reduce symptoms.
- Pain relievers: Over-the-counter pain relievers are often used to treat headaches; however, a doctor may prescribe higher doses for migraines. Do not exceed the suggested dose, and do not rely on them if you have more than 10 attacks a month. Even over-the-counter pain medicines can cause rebound headaches in migraine sufferers.
- Triptans: These medications target serotonin receptors and should be taken as soon as a migraine is noticed. They usually offer relief in 30-60 minutes, although they might aggravate nausea.
- Ditans: Some of these medications prevent attacks and are administered as injections or tablets. They inhibit CGRP molecules or receptors, preventing the chemical from flooding the brain during an attack. They typically have minor side effects, mostly discomfort at the injection site and constipation. These can be successful in reducing the intensity and frequency of migraines that you may only require an over-the-counter painkiller during an attack.
- Preventive medications: Birth control pills, antidepressants, and anti-seizure drugs
- Botox injections: Botox is approved for chronic migraine sufferers and works best for those with many headaches each month. Shots are administered around the head, neck, and shoulders to inhibit pain receptors in those muscles and nerves, stopping them from transmitting signals to the brain. There are some rare adverse effects, but the most common side effect is a temporary headache following the injections. Botox shots are generally given when other treatments do not provide relief.
- Neuromodulation: You can try a pulsing device that sends electrical signals to the nerves to suppress migraine discomfort.
How can lifestyle changes help with migraines?
Doctors frequently recommend the following lifestyle changes to help with migraines:
- Getting quality sleep: Migraine sufferers often have difficulty falling or staying asleep, and sleep deprivation can trigger more migraine attacks. Treating sleep disorders such as sleep apnea may help you get better sleep.
- Eating healthy: Poor diet and obesity have been linked to chronic migraines. Try to eat more plant-based foods and avoid processed, sugary foods.
- Manage stress: Meditation, yoga, and other relaxation techniques can help reduce stress and prevent the frequency of migraine attacks.


