Contents
Endoscopic Ultrasound (EUS)
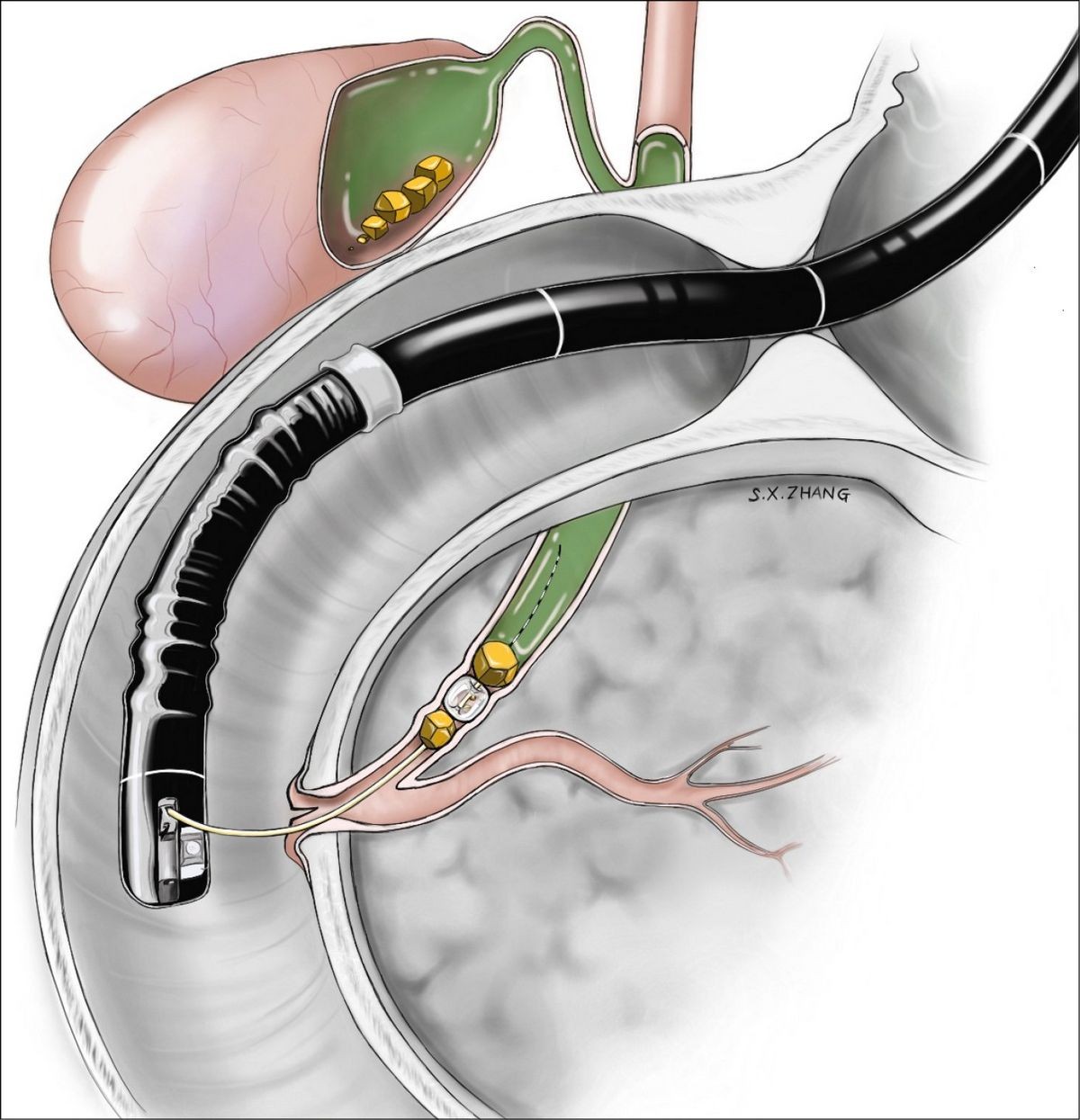
Endoscopic Ultrasound (EUS) combines endoscopy and ultrasound to obtain images and information about the digestive tract and surrounding tissue and organs. Endoscopy involves inserting a long flexible tube via the mouth or the rectum to visualize the digestive tract. Ultrasound, on the other hand, uses high-frequency sound waves to produce images of the organs and structures inside the body, including the ovaries, uterus, liver, gallbladder, pancreas, or aorta.
Traditional ultrasound uses a transducer placed on the skin overlying the organ(s) of interest, but the images obtained are not always of high quality. In EUS, a small ultrasound transducer is installed on the tip of the endoscope, allowing for high-quality ultrasound images of the organs inside the body.
The proximity of the EUS transducer to the organ(s) of interest results in frequently more accurate and detailed images compared to traditional ultrasound. EUS can also provide information about the layers of the intestinal wall, as well as adjacent areas such as lymph nodes and blood vessels.
EUS has additional uses, including studying blood flow inside blood vessels using Doppler ultrasound and obtaining tissue samples through fine needle aspiration (FNA) under ultrasound guidance. These samples can be examined by a pathologist under a microscope for further analysis.
When is EUS useful?
EUS is utilized in various situations, including:
- Staging cancers of the esophagus, stomach, pancreas, and rectum.
- Staging lung cancer.
- Evaluating chronic pancreatitis and other masses or cysts of the pancreas.
- Studying bile duct abnormalities, including stones and tumors.
- Assessing the muscles of the lower rectum and anal canal in evaluating fecal incontinence.
- Detecting submucosal lesions in the intestinal wall.
EUS plays an important role in cancer staging, providing information about the depth of penetration and spread of cancer. This information is crucial for determining the prognosis and appropriate treatment options.
QUESTION
What is the preparation for EUS?
Prior to EUS, it is important to provide your doctor with relevant health information, including any allergies or significant health problems. Your doctor may also inquire about allergies to iodine or shellfish, as iodine-containing contrast material may be used in certain circumstances. A blood clotting test may be necessary if fine needle aspiration (FNA) is a possibility. It is important to disclose any family history of bleeding problems or medications that affect blood clotting. Antibiotics are generally unnecessary, unless certain heart valve problems are present.
EUS is performed under sedation, requiring you to refrain from driving or returning to work for 24 hours. It is necessary to arrange for someone to accompany you home after the outpatient procedure.
You will need to have an empty stomach, fasting for 6 or more hours. Additional instructions, including the use of enemas or laxatives, may be provided depending on the specific procedure.
How is EUS performed?
Upon arrival at the endoscopy center, you will receive information about the procedure and have an opportunity to ask questions. You will be asked to sign a consent form after understanding the procedure, its alternatives, and associated risks. Following the administration of sedation, the EUS will be performed. Monitoring equipment will be attached to track your pulse, blood pressure, and blood oxygen levels.
During the procedure, the special endoscope will be inserted, and the physician will observe the inside of your intestinal tract on a TV monitor, as well as the ultrasound image on another monitor. The entire procedure typically lasts between 30 and 90 minutes, depending on complexity and whether fine needle aspiration (FNA) is performed.
After the procedure, you will experience drowsiness for up to one hour and will be advised not to drink or walk. Once fully awake, the doctor will discuss the findings with you and your companion, if desired. Rare complications aside, you will be able to return home to rest for the remainder of the day. Light meals and fluids are allowed. Temporary bloating may occur due to the use of carbon dioxide to distend the abdomen. Salt-water gargles can help alleviate mild throat soreness. If you have concerns or experience severe pain, vomiting, or other abnormal symptoms, it is important to contact your doctor. In some cases, hospitalization overnight may be required, and this will be discussed by the endoscopist.
What are the risks of EUS?
EUS is generally safe and well tolerated. However, like any medical procedure, it is not without risk. Complications with EUS are rare, occurring at a rate of approximately one in two thousand procedures. Reactions to medications used during EUS, such as hives, skin rash, or nausea, can occur. A lump may develop at the site of the IV placement, but this usually resolves over time. If it persists, it is advisable to contact your physician. Perforation of the intestinal wall is a rare but serious complication that may require surgical repair, and strict precautions are taken to prevent it.
When fine needle aspiration (FNA) is performed, complications occur more frequently but are still uncommon, with a rate ranging from 0.5% to 1.0%. Minor bleeding may occur when passing a needle through the gut wall, and in rare cases, hospitalization may be required for observation. Infection is another rare complication, which can be minimized by administering antibiotics before the procedure. Pancreatitis, inflammation of the pancreas, is a rare occurrence when FNA is performed on the pancreas. It may call for hospitalization, abdominal pain medication, and rest, but typically resolves within a few days.