Can Vulvar Cancer Be Cured?
When vulvar cancer is detected and treated early, the cure rate is greater than 90 percent. The key to a cure is to notify your doctor as soon as you notice any warning signs and to have a biopsy performed as soon as possible.
Vulvar cancer affects less than one percent of women. While it is uncommon, it is very treatable, especially in the early stages.
- Vulvar cancer is a slow-growing tumor that usually develops over several years.
- For a long time, precancerous cells can grow on the surface of the vulvar skin. The term for this precancerous condition is vulvar intraepithelial neoplasia (VIN) or dysplasia.
- VIN is nearly completely curable. Almost all patients with vulvar cancer that has not spread to the lymph nodes live for at least five years.
- Because VIN or dysplasia can progress to vulvar cancer, treatment for this condition is critical.
- If vulvar cancer has spread to the lymph nodes, the prognosis is determined by the number of lymph nodes affected.
Contents
Outlook for vulvar cancer
- The prognosis for vulval cancer is determined by factors, such as how far your cancer has spread, age, and overall health.
- In general, approximately 6 out of 10 women diagnosed with vulval cancer will live for at least five years from the time of diagnosis (five-year survival).
- Even after successful treatment, cancer can reoccur in up to one out of every three cases. You will need to see your doctor regularly to see if this is happening.
- In the United States, a woman has a 1/333 chance of developing it, which accounts for 6,000 cases per year.
- The five-year survival rate of cancer that has not spread to lymph nodes is greater than 80 percent.
- Survival is less than 50 percent after five years if inguinal nodes are involved, and only 10 to 15 percent if other nodes are involved.
- Patients older than 80 years are generally diagnosed at a later stage. Less aggressive treatments generally have a lower success rate.
Treatment options for vulvar cancer
Vulvar cancer typically develops over many years, but it is easier to treat at an early stage. Treatment may include:
- Surgery
- Radiation therapy
- Chemotherapy
- Combination treatment
Your doctor’s treatment plan will be based on the results of your tests, the type of cancer, where the cancer is located, whether it has spread, your age, and your overall health.
You will be checked regularly to see if cancer has responded to treatment.
Surgery
The goal of surgery is to remove cancer from the vulva while preserving as much normal tissue as possible.
- Laser surgery: Instead of a scalpel, specialists use a laser beam to make cuts in tissue or to remove a surface lesion or tumor.
- Wide local excision: It involves the removal of cancer and a clear margin of normal tissue around it.
- Radical local excision: When the cancer is more advanced, the surgical procedure to remove it may necessitate the removal of a large amount of normal tissue around it, as well as nearby lymph nodes in the groin.
- Vulvectomy: A vulvectomy is a surgical procedure that removes a portion of the entire vulva.
- Surgical aspiration using ultrasound: The doctor may use fine sound vibrations to break up the tumor into small pieces during this surgical procedure. The small pieces of the tumor are washed away and suctioned out. This procedure causes less damage to the surrounding tissue.
- Pelvic exenteration: This surgery is reserved for patients with advanced-stage vaginal cancer (stage IV) or who have had a recurrence of their vaginal cancer despite conventional treatment. Pelvic exenteration surgery involves the removal of the lower colon, rectum, and bladder. The cervix, vagina, ovaries, and nearby lymph nodes are also removed. To allow urine and stool to flow from the body into a collection bag, artificial openings (stomas) are created on the abdomen.
Even if the doctor removes all visible cancer during the surgery, some patients may require additional chemotherapy or radiation therapy to kill any cancer cells that remain.
Radiation therapy
Radiation therapy is a type of cancer treatment that uses high-energy X-rays or other types of radiation to either kill or prevent cancer cells from growing.
Radiation therapy is classified into two types.
- External radiation therapy directs radiation to cancer using a machine located outside the body.
- Internal radiation therapy, also called brachytherapy, involves the use of a radioactive substance that is sealed in needles, seeds, wires, or catheters that are inserted directly into or near cancer.
Chemotherapy
- Chemotherapy is a cancer treatment that employs medicines to halt the growth of cancer cells, either by killing them or preventing them from dividing.
- Chemotherapy drugs enter the bloodstream and can affect cancer cells throughout the body when taken orally or injected into a vein or muscle.
- Topical chemotherapy, in the form of a cream or lotion, may sometimes be applied to the vagina.
Immunotherapy
- This type of cancer treatment employs your immune system to combat the disease.
- Immunotherapy uses substances produced by your body or created in a laboratory to boost, direct, or rebuild the body’s natural anti-cancer defenses.
- Imiquimod is an immunotherapy that is applied to the skin in the form of a cream to treat vulvar lesions.
Side effects of vulvar cancer treatments
There may be some treatment complications you experience once the treatment is finished, which are:
- Change in bowel patterns
- Infections
- Changes in skin color around the vulva
- Abnormal urination
- Discomfort during sexual intercourse
- Fatigue and weakness
- Upset stomach
- Diarrhea, nausea, and vomiting
- Low blood counts
- Mouth or vaginal sores
- Temporary hair loss
- Reduction of sexual desire or pleasure
What is vulvar cancer?
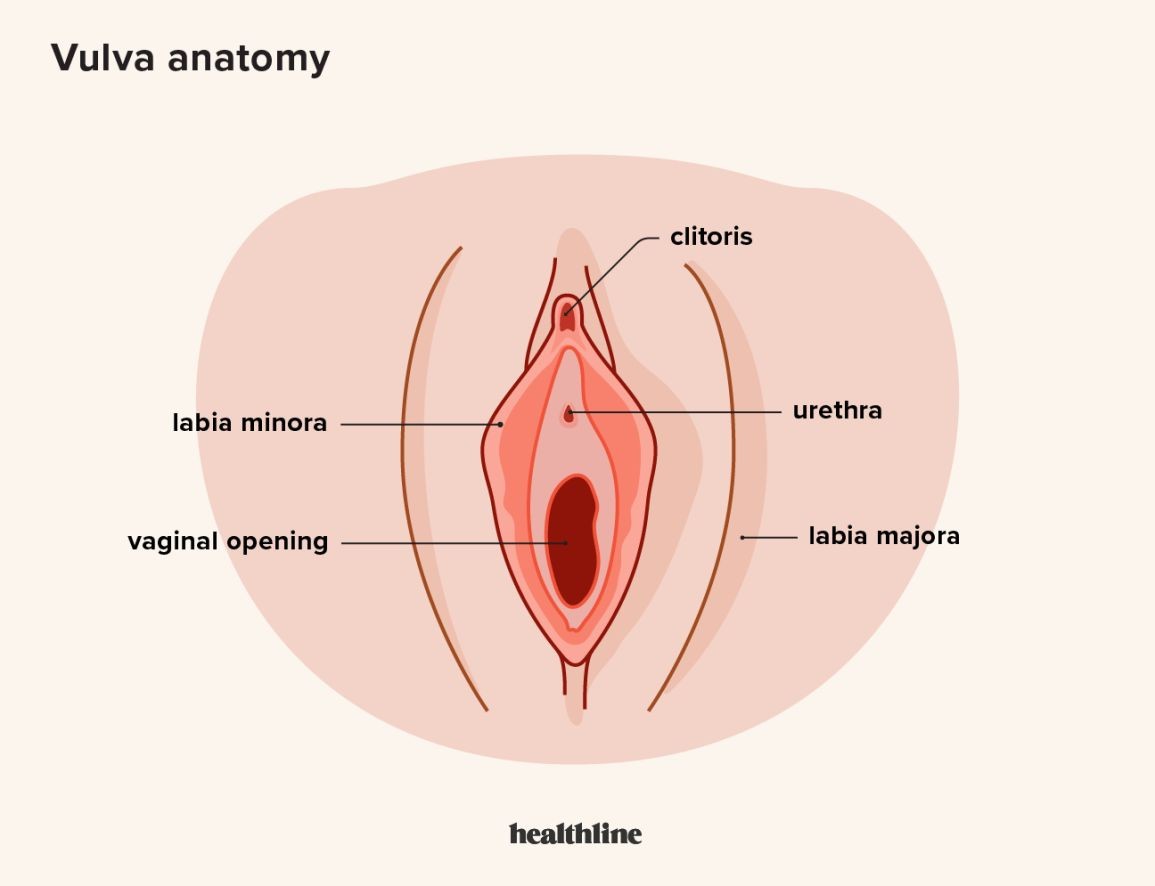
Vulvar cancer is characterized by the abnormal growth of malignant cells in the vulva, which contains:
- Inner and outer vaginal lips
- The clitoris
- The vaginal opening
- The vaginal glands
Vulvar cancer is a rare type of cancer that occurs when cancerous cells develop in any part of the vulva.
Common symptoms of vulvar cancer
Itching around the vaginal area is common in women with this condition and can last for years.
Other skin changes that may occur in the vicinity of the vulva are:
- Mole or freckle , which may be pink, red, white, or gray
- Skin thickening or lump
- Pain or burning with urination
- Pain with intercourse
- Unusual odor
- Wart-like bumps, cauliflower-like growths or ulcers, or sores on the vulva that last more than a month
- Burning or bleeding and discharge not related to your menstrual cycle
- Enlarged lymph glands in your groin
What are the risk factors of vulvar cancer?
Although the specific cause of vulvar cancer is unknown, some risk factors appear to enhance your chances of developing the condition, including:
- Increasing age: Vulvar cancer risk increases with age although it can occur at any age. The average age at diagnosis is 65 years.
- Being exposed to human papillomavirus (HPV):HPV infection raises the risk of a variety of cancers, including vulval and cervical cancer. Many young, sexually active people are infected with HPV, but the infection usually resolves on its own. For some, the infection causes cell changes, increasing their risk of developing cancer in the future.
- Smoking cigarettes:Cigarette smoke consists of many cancer-causing chemicals. Both passive and active smoking can increase the risk of several cancers including vulval cancer.
- Having a weakened immune system: People who take immunosuppressive medications, such as those who have had organ transplants and those who have immunosuppressive conditions, such as human immunodeficiency virus (HIV), are at a higher risk of developing vulval cancer.
- Having a history of precancerous conditions of the vulva: A small number of vulvar intraepithelial neoplasia cases may progress to invasive vulvar cancer. As a result, your doctor may advise treatment to remove the abnormal cells and periodic follow-ups.
- Having a skin condition involving the vulva: Lichen sclerosus, which causes thin and itchy vulval skin, raises the risk of vulval cancer.
Tests to diagnose vulvar cancer
- X-ray of the chest: Done to see if cancer has spread to the lungs.
- Computed tomography scan: Done to detect large vulvar tumors or enlarged lymph nodes.
- Magnetic resonance imaging: Used to identify pelvic tumors and enlarged lymph nodes in the groin. This test may not be required in patients with early vulvar cancer.
- Positron emission tomography scan: This test generates three-dimensional images of the internal organs of the body. This test can detect cancer cells and determine whether cancer has spread to lymph nodes.
- Sentinel node biopsy: A dye is injected near the tumor, and it travels to the lymph nodes via the lymph vessels. Sentinel node detection has increased to 95 percent or higher due to the dyes that make the nodes glow under special goggles. International trials are being led by researchers to validate the role of sentinel node biopsy in vulvar cancer.
Precancerous conditions on the vulva may be detected during a routine annual visit to the gynecologist before the onset of symptoms. Self-examination in front of a mirror may also aid in the early detection of vulvar abnormalities.
Any new findings, especially raised, whitish, hyper-pigmented, or painful ulcers should be immediately reported to your doctor.
What Is Polycythemia Vera?


