Contents
Bile Duct Cancer (Cholangiocarcinoma)
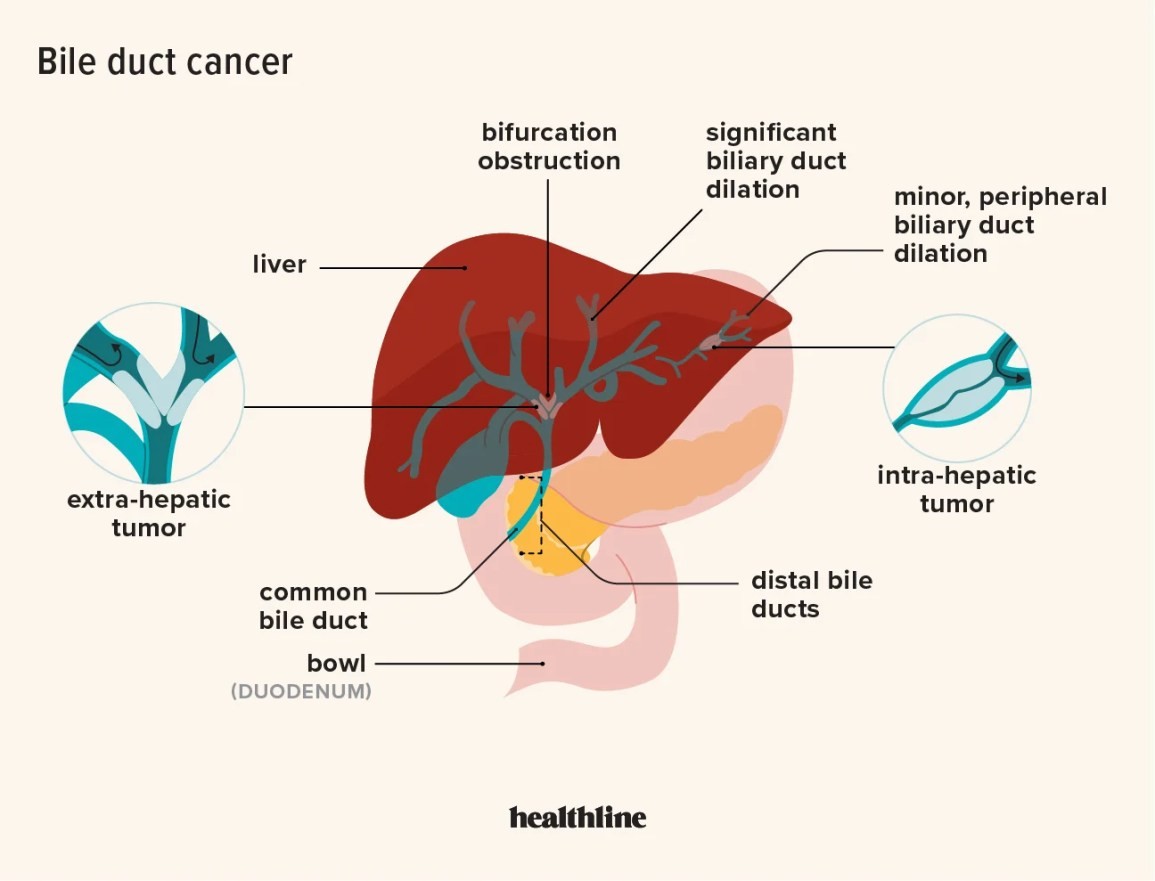
Bile duct cancer arises from the cells that line the bile ducts, the drainage system for bile produced by the liver. Bile ducts collect this bile, draining it into the gallbladder and finally into the small intestine where it aids in digestion. Bile duct cancer is also known as cholangiocarcinoma.
Bile duct cancer is an uncommon form of cancer, with approximately 8,000 new cases diagnosed in the United States each year. There are three general locations where this cancer may arise within the bile drainage system:
- Within the liver (intrahepatic) affecting the bile ducts located within the liver
- Just outside of the liver (extrahepatic or perihilar) located at the notch of the liver where the bile ducts exit
- Far outside of the liver (distal extrahepatic) near where the bile ducts enter the intestine (ampulla of Vater)
Bile duct cancers are most commonly found just outside of the liver in the perihilar area and least commonly found within the liver.
What are the statistics for bile duct cancer?
Approximately 8,000 new cases of bile duct cancer are diagnosed each year in the United States. The average age at diagnosis for people with intrahepatic bile duct cancer is 70. For extrahepatic bile duct cancer, the average age at diagnosis is 72.
What are causes and risk factors for bile duct cancer?
Depending on where the bile duct blockage occurs, this can lead to inflammation of the liver (hepatitis) and/or pancreas (pancreatitis).
The incidence of bile duct cancer increases with age. It is a slow-growing cancer that invades local structures and for that reason, the diagnosis is often made late in the disease process when the bile ducts become blocked. This blockade prevents bile drainage from the liver into the gallbladder and intestine. Depending on where the blockage occurs, this can lead to inflammation of the liver (hepatitis) and/or pancreas (pancreatitis).
The cause of bile duct cancer in most people is not understood. However, chronic inflammation of the bile ducts may be a risk factor for this cancer. Diseases that can cause chronic inflammation include primary sclerosing cholangitis (especially when associated with ulcerative colitis), chronic liver disease (including hepatitis B, hepatitis C, chronic alcoholic hepatitis, and cirrhosis).
Certain parasitic infections found in the Far East that cause liver infections are also associated with an increased risk.
Gallstones are not a risk factor for developing bile duct cancer, but stones within the liver do pose an increased risk. Liver stones are not often seen in the North American population but are more common in Asian countries.
There are rare congenital diseases that increase the risk of bile duct cancer, including Lynch II syndrome (hereditary nonpolyposis colorectal cancer associated with biliary tree and other cancers) and Caroli’s syndrome (portal hypertension, hepatic fibrosis, and biliary tree cysts).
Native Americans are six times more likely to develop bile duct cancer. Asian Americans may also be at higher risk. Bile duct cancer is also more prevalent in Israel and Japan but is very rare in North America.
What are bile duct cancer symptoms and signs?
The initial symptoms of bile duct cancer are jaundice, itching, abdominal pain, bloating, and weight loss.
The initial symptoms of bile duct cancer occur because of the inability of bile to drain normally from the liver where it is produced. This causes liver inflammation (hepatitis). Symptoms of cholangiocarcinoma include yellow coloring of the skin and eyes (jaundice), itching, abdominal pain, bloating, and weight loss. There may also be a low-grade fever, darkening of urine and stool.
Unfortunately, bile duct tumors may not cause any symptoms until they have grown in size and cancer has spread (metastasized) from its original location. Abdominal pain is often a late symptom and is usually located in the right upper quadrant and may be associated with a tender, enlarged liver.
QUESTION
How is bile duct cancer diagnosed?
History and physical examination are key clues for the diagnosis of bile duct cancer. Painless jaundice may be the only initial clue. The history often includes reviewing alcohol use, drug use, or recent illnesses associated with hepatitis or liver inflammation. Other symptoms of cholangiocarcinoma may include weight loss, loss of appetite, weakness, loss of energy, easy bruising or bleeding (factors that clot the blood are manufactured in the liver and loss of liver function may decrease blood clotting factors).
The physical examination may be useful in detecting tenderness in the abdomen, especially in the right upper quadrant beneath the ribs (where the liver is located). A quarter of patients with bile duct cancer will have an enlarged liver that can be palpated. During a general exam, the patient is often jaundiced, having yellow-tinged skin, which can be seen most easily in the white portion of the eyes or under the tongue.
Blood tests are often ordered to assess liver function. Liver enzymes, bilirubin levels, complete blood count, electrolytes, BUN and creatinine, and INR/PTT and PT are commonly performed.
There is no blood test that can specifically diagnose bile duct cancer. The diagnosis is confirmed by a tissue sample obtained by biopsy by a surgeon, gastroenterologist, or interventional radiologist and a pathologist using a microscope to examine the cells obtained from the biopsy sample.
Imaging may be used to evaluate the structure of the liver, gallbladder, bile ducts, and other surrounding organs. Tests like ultrasound, CT scan, and MRI may be performed to look for a tumor and its location.
Endoscopic retrograde cholangiopancreatography (ERCP) is a specialized test used to examine the bile duct as it enters the duodenum. ERCP is performed by a gastroenterologist using a fiberoptic camera at the end of a flexible viewing tube. The tube is passed through the mouth and threaded through the stomach into the first part of the small intestine where the common bile duct enters. This test is commonly performed to examine the lining of the esophagus and stomach but is also effective in detecting conditions that affect the bile ducts, including bile duct cancer, gallstones stuck in the bile duct, and abnormal narrowing of the bile duct. Dye can be injected through the tube into the bile duct opening to outline the bile ducts and detect obstruction. Biopsies or cell washings can be obtained to look for cancer cells. If a blockage is found, a stent may be placed to keep the duct open and allow bile to drain.
Sometimes, an interventional radiologist may obtain a tissue biopsy by threading a needle through the skin into the liver.
Once the diagnosis of bile duct cancer is made, it is important to stage the cancer to help direct potential treatment. The three parts of TNM staging include the following:
- T is for the primary tumor and how much it has grown locally and invaded other structures. For a bile duct tumor, this includes the liver, gallbladder, pancreas, stomach, and intestine.
- N is for the lymph nodes that are involved. The more nodes involved and the farther the distance from the bile duct, the more severe the cancer.
- M is for metastasis. Has the tumor spread to other parts of the body?
Cancer can be staged from 0 to 4, where 0 is a precancerous condition, 1 is a local tumor with no spread to lymph nodes or other parts of the body, and 4 is significant local growth and lymph node involvement and spread to other parts of the body.
While staging is important, as well as detecting tumor spread beyond the liver and bile duct, often the critical staging questions can only be answered at surgery. During an operation, the surgeon can decide whether or not the entire tumor can be resected. Survival rates are significantly improved if complete resection is possible.
What Is Polycythemia Vera?
What Is Polycythemia Vera?