Contents
What are the 5 Warning Signs of a Stroke?
Strokes can cause brain damage and death. However, the acronym F.A.S.T. is a great way to remember stroke symptoms.
A stroke—also called a cerebrovascular accident (CVA) or brain accident—happens when a blood clot travels to the brain or when a brain blood vessel bursts. Strokes can cause brain damage and death. However, learning the warning signs of a stroke can lead to early medical intervention, which leads to a better outcome in some people.
Signs of a stroke
The acronym F.A.S.T. is a great way to remember stroke symptoms.
1. F – Face drooping
One side of the face drooping is a sign of a stroke. If the face is numb, that may also be a sign. To tell for sure, ask the person to smile. If the smile is lopsided, they may be having a stroke.
2. A – Arm weakness
Ask the person to lift both arms. If one arm is weaker and drifts down, they may be having a stroke. Numbness or weakness on one side of the body is a common stroke symptom.
Slurred speech or difficulty talking coherently may be a sign of stroke. Say a simple sentence like: "The sky is blue today." If the person has trouble repeating it, they may require medical attention.
When someone is having a stroke, time is of the essence. If you suspect a stroke, get medical attention right away. Call 911 or take them to the nearest emergency department immediately.
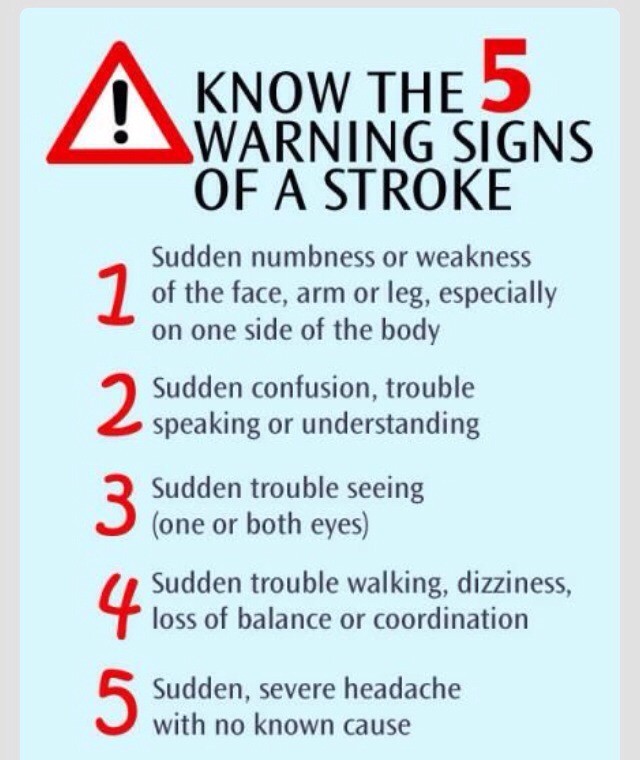
Overall, the five biggest warning signs of a stroke are:
- Weakness or numbness on one side of the body
- Difficulty talking
- Sudden changes in vision
- Sudden difficulty walking
- A sudden severe headache
Other signs of stroke include:
- Confusion
- Feeling dizzy
- Lack of balance or stability
Types of stroke
Ischemic stroke
87% of strokes are ischemic. A blockage of the arteries that bring blood to the brain causes an ischemic stroke. This is usually caused by a blood clot. Trauma to the blood vessel can also cause one.
Hemorrhagic stroke
During a hemorrhagic stroke, a blood vessel in the brain leaks or tears. Blood then pools and puts pressure on the brain, leading to damage. High blood pressure and aneurysms usually cause hemorrhagic strokes.
Transient ischemic attack (TIA)
Also called a mini-stroke, this type of stroke occurs for fewer than five minutes and may not cause as much damage. Even so, they are a major warning sign for major strokes and are still a medical emergency.
At the beginning of a stroke, you don’t know whether it will be a mini-stroke or a major one, so it’s important to call 911 or bring the person to the nearest emergency department immediately.
Over 33% of people who have a TIA will have a major stroke within the next year. Up to 15% of people who have a TIA will have a major stroke in the next three months.
Causes of stroke
Strokes are caused by:
- Blood clots blocking arteries to the brain
- Trauma to brain arteries
- Rupture of brain arteries
- Leakage in brain arteries
However, several conditions lead to a higher risk for a stroke.
High blood pressure
Many people with high blood pressure have no symptoms. Yet, it is one of the leading causes of a stroke. The best way to find out if you have high blood pressure is to check it often. If you do have high blood pressure, follow your doctor’s recommendation for lifestyle changes or prescription medication to reduce your risk of stroke.
High cholesterol
Excess cholesterol from our diet can build up in arteries and veins, leading to sclerosis—narrowing of the arteries—and blockages.
Heart disease
The same things that cause heart disease are also risk factors for stroke. So, if you have heart disease, you may also be at a higher risk for a stroke.
Sickle cell disease
In this blood disorder, some red blood cells are sickle-shaped. This shape is more likely to get stuck in blood vessels, leading to a stroke.
Previous strokes or mini-strokes
Those who have already had a stroke or mini-stroke have a higher risk of having another one.
Diagnosis for stroke
If you have stroke symptoms, doctors will perform several tests and exams to diagnose you. They may:
- Take a detailed medical history
- Perform a physical exam
- Perform a neurological exam
- Order blood tests
- Order a CT scan, MRI, X-ray, or other brain imaging
- Use an electroencephalogram (EEG) to show the brain’s electric impulses
- Perform an ultrasound test to find artery blockages
Treatments for stroke
Emergency treatment
Experts say that time is of the essence when it comes to strokes. The faster you get to the hospital, the better outcome you may have. Those who take an ambulance to the hospital may get a faster diagnosis and thus, faster treatment.
If you arrive at a hospital within three hours of your first stroke symptoms, and you have an ischemic stroke, you will likely receive a "clot-busting" medication known as a thrombolytic. This breaks up blood clots, allowing blood flow to return to normal. People who get this treatment have less brain damage and are less likely to require long-term care after a stroke.
In the case of a hemorrhagic stroke, doctors may repair the leaking or ruptured artery via an endovascular procedure. They insert a long instrument through one of the major arteries in the arm or leg. They use the instrument to install a device to repair the artery or stop the bleeding. Some hemorrhagic strokes require surgery.
Rehabilitation
After a stroke, most people need some kind of rehabilitative treatment. However, this treatment is different for each person, depending on the severity of the stroke and brain damage. The goal of rehabilitation is to help people who have had a stroke live as independently as possible.
Ten percent of people who have had a stroke will require long-term care. Another ten percent will recover completely. Most people fall somewhere in the middle, with minor to moderate impairments.
Rehabilitation treatment may occur in:
- The hospital
- A rehabilitation facility
- A long-term care facility
- At home
- An outpatient facility
After having a stroke, you may work with a variety of doctors and medical professionals to help with rehabilitation. Some of these people will help you with future stroke prevention, and others help you regain function and improve impairments. Some people you may work with include:
- Physical therapist
- Rehabilitation nurse
- Occupational therapist
- Speech-language pathologist
- Social worker
- Dietitian
- Neuropsychologist
- Case manager
- Recreational therapist
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet, and I understand that I may opt out of MedicineNet subscriptions at any time.
American Stroke Association: "Common Diagnosis Methods."
American Stroke Association: "Rehab Therapy After a Stroke."
American Stroke Association: "Stroke Symptoms."
Beaumont: "Stroke Symptoms: From FAST to FASTER."
Centers for Disease Control and Prevention: "About Stroke."
Centers for Disease Control and Prevention: "Conditions That Increase Risk for Stroke."
Centers for Disease Control and Prevention: "Stroke Treatment."
Centers for Disease Control and Prevention: "Types of Stroke."
The Internet Stroke Center: "Ischemic Stroke."
Medline Plus: "Stroke."
UC San Diego Health Neurological Institute: "Warning Signs and Risk Factors for Stroke."
American Stroke Association: "Common Diagnosis Methods."
American Stroke Association: "Rehab Therapy After a Stroke."
American Stroke Association: "Stroke Symptoms."
Beaumont: "Stroke Symptoms: From FAST to FASTER."
Centers for Disease Control and Prevention: "About Stroke."
Centers for Disease Control and Prevention: "Conditions That Increase Risk for Stroke."
Centers for Disease Control and Prevention: "Stroke Treatment."
Centers for Disease Control and Prevention: "Types of Stroke."
The Internet Stroke Center: "Ischemic Stroke."
Medline Plus: "Stroke."
UC San Diego Health Neurological Institute: "Warning Signs and Risk Factors for Stroke."


