Contents
- 1 Temporomandibular Joint Syndrome (TMJ)
- 1.0.1 What causes TMJ syndrome?
- 1.0.2 What are the risk factors for TMJ syndrome?
- 1.0.3 What are signs and symptoms of TMJ syndrome?
- 1.0.4 What types of doctors diagnose and treat TMJ syndrome?
- 1.0.5 How do healthcare professionals diagnose TMJ syndrome?
- 1.0.6 What is the best treatment for TMJ syndrome?
- 1.0.7 What is the prognosis for TMJ syndrome?
Temporomandibular Joint Syndrome (TMJ)
Temporomandibular joint (TMJ) syndrome is a disorder of the jaw muscles and nerves caused by injury or inflammation of the temporomandibular joint. The temporomandibular joint is the connection between the jawbone and the skull. The injured or inflamed temporomandibular joint leads to:
- Pain with chewing, clicking, crackling, and popping of the jaw
- Swelling on the sides of the face
- Nerve inflammation
- Headaches, including migraines
- Tooth grinding (bruxism)
- Eustachian tube dysfunction
- Dislocation of the temporomandibular joint
A temporomandibular joint syndrome is also known as a temporomandibular joint disorder.
What causes TMJ syndrome?
Medical professionals do not completely understand the causes of TMD. Multiple factors contribute to the muscle tightness and dysfunction that characterize this condition. It is not clear whether some of these causes directly lead to TMJ syndrome or if they are a result of the disorder.
Causes of TMJ syndrome may include:
- Misalignment (malocclusion) of or trauma to the teeth or jaw
- Teeth grinding (bruxism)
- Poor posture
- Stress or anxiety
- Arthritis and other inflammatory musculoskeletal disorders
- Orthodontic braces
- Excessive gum chewing
What are the risk factors for TMJ syndrome?
Several risk factors for TMD include:
- Poor posture in the neck and upper back muscles may lead to neck strain and abnormalities of jaw muscle function.
- Stress may increase muscle tension and jaw clenching.
- Women 18-44 years of age have increased risk.
- Patients with other chronic inflammatory arthritis have increased risk.
- People with jaw trauma or poorly positioned teeth have increased risk.
- People who have a genetic predisposition to pain sensitivity and increased stress responses may be more susceptible.
What are signs and symptoms of TMJ syndrome?
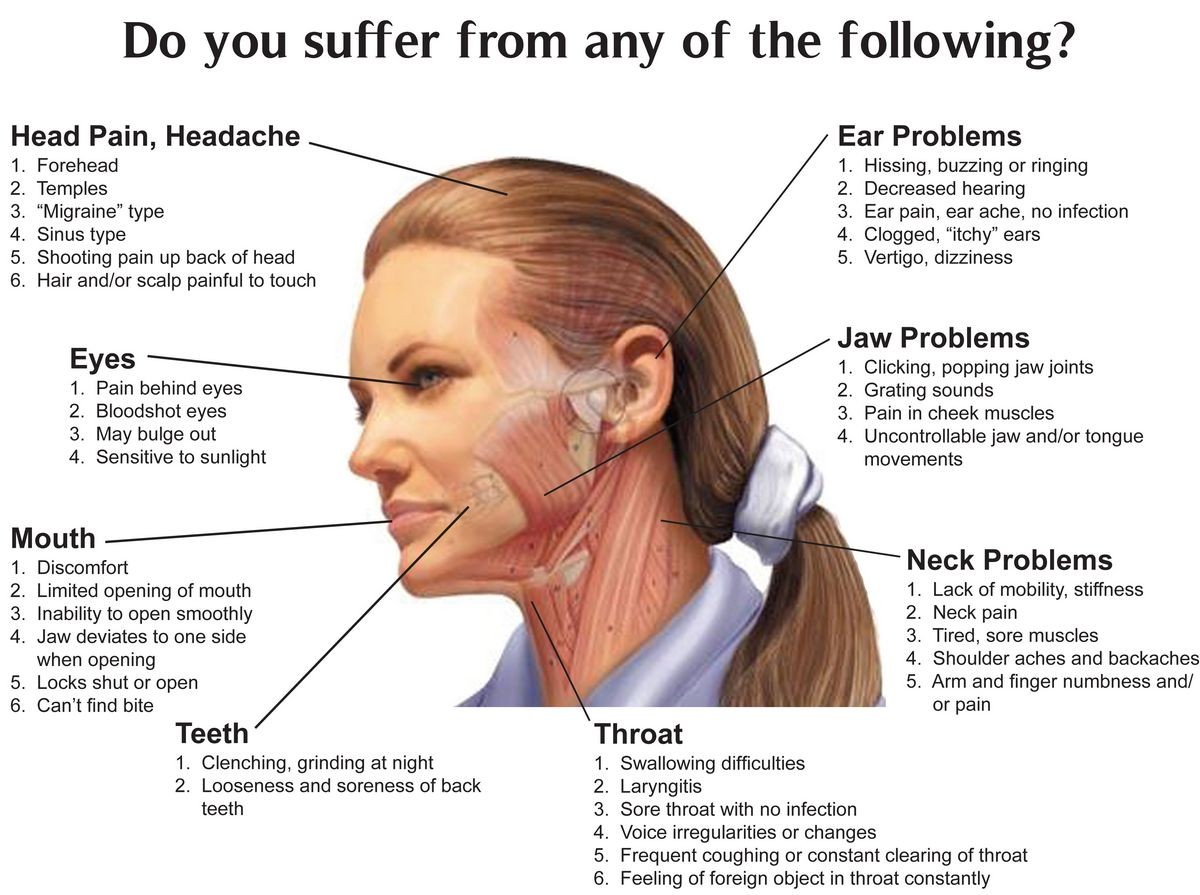
The main TMD symptom is pain in the jaw joint. This joint is located just in front of the ear, and pain associated with TMD may involve the face, eye, forehead, ear, or neck.
Signs and symptoms of temporomandibular joint dysfunction include:
- Pain or tenderness in the jaw, especially in the area of the joint
- Popping/clicking of the jaw (crepitus)
- Pain that feels like a toothache
- Ear pain (earache) or sounds of cracking in the ears
- Ringing or popping sounds in the ears (tinnitus) or a sense of fullness in the ears
- Headaches, including migraines
- Blurred vision
- Tight, stiff, or sore jaw or neck muscles
- Muscle spasms in the jaw
- Facial pain, mouth pain, jaw pain, cheek pain, or chin numbness or tingling
- Pain at the base of the tongue
- Pain, swelling, or a lump in the temple area
- Difficulty chewing
- Shoulder pain
- Locking or dislocation of the jaw (usually after widely yawning), referred to as lockjaw
- Dizziness or vertigo
What types of doctors diagnose and treat TMJ syndrome?
A primary care provider (PCP), such as a family practitioner, internist, or a child’s pediatrician, may first diagnose your TMJ. Your doctor may refer you to an oral and maxillofacial specialist, an otolaryngologist (also called an ear, nose, and throat doctor or ENT specialist), or a dentist specializing in jaw disorders (prosthodontist, also called a prosthetic dentist) for further treatment. You may also see a pain-management specialist if your TMJ pain is severe.
How do healthcare professionals diagnose TMJ syndrome?
A doctor will diagnose TMD by taking the patient’s medical history and doing a physical exam to find the cause of the symptoms. There is no specific test to diagnose TMD. A doctor may send the patient to an oral and maxillofacial specialist, an otolaryngologist (also called an ear, nose, and throat doctor or ENT specialist), or a dentist specializing in jaw disorders to confirm the diagnosis. Sometimes a healthcare professional may order an MRI of the temporomandibular joint to detect damage to the cartilage of the jaw joint and to rule out other medical problems.
A condition that may have some similar symptoms to TMD is trigeminal neuralgia. The trigeminal nerve supplies nerve impulses to the temporomandibular joint, and when irritated, it can cause facial pain. Other causes of face or neck pain include swollen lymph nodes (swollen glands), giant cell arteritis, salivary gland disease, sore throat, ill-fitting dentures, or dental braces.
QUESTION
What is the best treatment for TMJ syndrome?
Many symptoms of TMJ disorders can respond well to home remedies or stress reduction and relaxation techniques. The best home remedies that may provide some relief are:
- Ice or cold packs to the area of the joint
- Over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin) or naproxen (Aleve), and other pain relievers, including aspirin (Ecotrin) and acetaminophen (Tylenol)
- Eating soft foods and avoiding chewing gum
- Massage or gentle self-stretching of the jaw and neck muscles (A doctor or physical therapist can recommend appropriate stretches.)
- Relaxation techniques and stress management and reduction
- Some sedative essential oils (such as lavender, chamomile, sweet marjoram, and clary sage) may provide temporary relief from the pain and discomfort of TMJ.
When home remedies are not effective, medical treatment options may be necessary. Most of these types of treatments and remedies will not cure TMD, but they can provide temporary and even long-term relief from the pain symptoms. The most common treatments include:
- A dental splint (occlusal splint or stabilization splint or bite guard), is a dental appliance placed in the mouth that keeps the teeth in alignment and prevents tooth grinding. This resembles a mouth guard and is usually prescribed and fitted by a jaw specialist.
- A medical professional may use Botox to relax the muscles of the jaw. However, this is not currently an FDA-approved treatment for TMD.
- Physical therapy with jaw exercises can strengthen muscles, and improve flexibility, and range of motion.
- In states where medical marijuana is legal, a physician may prescribe it to help with severe TMJ pain.
- Biobehavioral management (biofeedback, cognitive-behavioral therapy [CBT]) may help diminish pain intensity.
- Trigger-point acupuncture can sometimes be helpful.
- In severe cases, surgery on the jaw or dental surgery may be necessary.
- TMJ arthroscopy or arthrocentesis is a minimally invasive procedure usually done in an outpatient setting. The recovery time for this procedure is about a week.
- Sometimes a total joint replacement may be necessary. This generally requires a stay in the hospital for several days, and surgery recovery time is four to six weeks.
What is the prognosis for TMJ syndrome?
The prognosis for TMJ syndrome is generally good. Numerous causes for TMJ syndrome exist, so the outlook depends on the cause if known. Most people can manage discomfort with self-care and home remedies.
Complications of long-term TMJ syndrome include chronic face pain or chronic headaches. In severe situations, where the pain is chronic or associated with other inflammatory disorders, long-term treatment may be necessary.
American College of Prosthodontists. "Temporomandibular Joint Disorder & Facial/Jaw Pain." .
"Study Evaluates Risk Factors for Chronic Temporomandibular Joint and Muscle Disorders." National Institute of Dental and Craniofacial Research. 10 Nov. 2011.
"TMJ." Amerian Academy of Otolaryngology – Head and Neck Surgery. Dec. 2010.
"TMJ Disorders." National Institute of Dental and Craniofacial Research. Aug. 2013.
"TMJ Disorders." National Institute of Dental and Craniofacial Research. Aug. 2013.


