Contents
- 1 Tardive Dyskinesia
- 1.0.1 How common is tardive dyskinesia?
- 1.0.2 What primarily causes tardive dyskinesia?
- 1.0.3 What drugs cause tardive dyskinesia?
- 1.0.4 Who is most likely to suffer from tardive dyskinesia?
- 1.0.5 What are the warning signs of tardive dyskinesia?
- 1.0.6 What is the difference between dystonia and tardive dyskinesia?
- 1.0.7 Akathisia vs. tardive dyskinesia
- 1.0.8 What specialists treat tardive dyskinesia?
- 1.0.9 How is tardive dyskinesia diagnosed?
- 1.0.10 Is there a test for tardive dyskinesia?
- 1.0.11 What are the treatment options for tardive dyskinesia?
- 1.0.12 Is medication for tardive dyskinesia available?
- 1.0.13 Are there natural remedies for tardive dyskinesia?
- 1.0.14 Is tardive dyskinesia reversible?
- 1.0.15 Can tardive dyskinesia be prevented?
- 1.0.16 What research for tardive dyskinesia is underway?
- 1.0.17 From
Tardive Dyskinesia
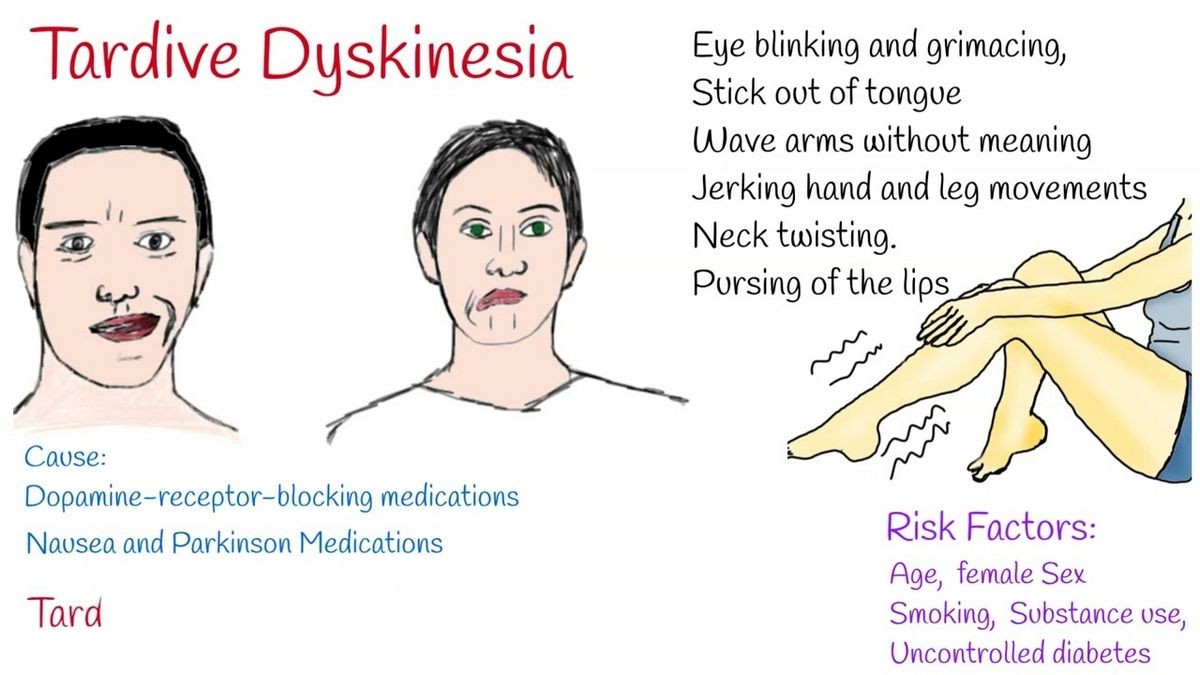
Dyskinesias are involuntary movements of the face (including lips, tongue, eyes), trunk, and extremities, identified in patients treated with certain dopamine-antagonist medications.
Dyskinesias are difficult to control. Various conditions can cause dyskinetic movements, including rheumatic fever, genetic disorders, and motor tics. Dyskinetic movements can include eye blinking or closure, mouth opening or lip pursing, involuntary tongue movements, or more pronounced movements of the extremities or trunk. Sometimes, dyskinetic movements can include sustained abnormal postures, called dystonia.
Tardive dyskinesias are a subgroup of dyskinesias that occur after exposure to certain types of medication. The most common medications that can lead to tardive dyskinesia include antipsychotic medications and medications used to treat chronic nausea. This class of medications is often used to treat psychiatric conditions such as schizophrenia, severe depression or anxiety, or bipolar disorder. These drug-induced movement disorders include orofacial dyskinesias, or involuntary movements of the mouth, eyes, and tongue.
How common is tardive dyskinesia?
The number of people who develop tardive dyskinesia is unknown, but estimates suggest that about 5%-6% of those who take neuroleptic or anti-nausea medications may develop symptoms; this number rises to about 25% of the elderly population. Sometimes tardive dyskinesia isn’t seen until the medication is stopped (this is called withdrawal dyskinesia); others find that their symptoms resolve after restarting the medication or adjusting the dose (this is known as "masked tardive dyskinesia").
What primarily causes tardive dyskinesia?
Although medications can trigger tardive dyskinesia, the underlying reason or cause remains unknown. Scientists speculate that medication-induced changes to a specific region in the brain (dopamine-2 or D-2 receptors) may lead to the movements, but this theory has not been proven.
What drugs cause tardive dyskinesia?
While antipsychotic medications, metoclopramide, and antiemetics have been implicated in the onset of tardive dyskinesia, the underlying cause remains unclear.
Who is most likely to suffer from tardive dyskinesia?
Risk factors for tardive dyskinesia include:
- Age
- Gender (older females are more likely to develop tardive dyskinesia, whereas younger males seem more likely to develop tardive dystonia)
- Duration of exposure to antipsychotic medications
- A dose of antipsychotic medications
- Cigarette smoking.
QUESTION
What are the warning signs of tardive dyskinesia?
There are many different symptoms associated with tardive dyskinesia, including:
- Twisting movements of the tongue or tongue protrusion
- Lip pursing or smacking
- Grimacing
- Cheek bulging or "puffing out"
- Chewing actions
- Eye closure
The facial movements may interfere with speaking or eating.
Other symptoms or signs include:
- Involuntary actions of the hands or feet, including persistent finger movements or toe extension
- Shoulder shrugging
- Neck movements (including pulling the head back or pushing it forward)
- Rocking activity
- Hip movements
- In rare cases, irregular breathing
Common symptoms of tardive dyskinesia
- Involuntary facial movements, especially tongue protrusion. In some cases, the tongue movements are so pronounced that the person’s tongue begins to grow, exacerbating the problems with protrusion.
- Lip pursing and grunting also are frequently identified in cases of tardive dyskinesia.
- Sometimes a person with tardive dyskinesia will appear to be chewing.
When the person is distracted, the movements are often worse; however, if the affected person becomes aware of the movements, he or she is often able to stop or decrease the activity.
What is the difference between dystonia and tardive dyskinesia?
When patients develop sustained twisting or abnormal postures related to medication use, a diagnosis of tardive dystonia may be made.
Akathisia vs. tardive dyskinesia
Akathisia is a sense of pronounced restlessness and an inability to sit still. People with akathisia will often pace, fidget, or march for hours on end. Unlike tardive dyskinesia, which occurs after several months or years of treatment, akathisia may arise after a single dose of a medication. Akathisia may be described as acute, occurring shortly after starting a medication, or tardive, occurring many months or years after starting the medication.
What specialists treat tardive dyskinesia?
Psychiatrists and neurologists, especially those who specialize in treating movement disorders, are most experienced in treating tardive dyskinesia.
How is tardive dyskinesia diagnosed?
Tardive dyskinesia is diagnosed after careful clinical examination and assessment of a patient’s history. Healthcare professionals consider and exclude other movement disorders, including drug-induced movement disorders, before making a diagnosis of tardive dyskinesia.
Is there a test for tardive dyskinesia?
Tardive dyskinesia is a clinical diagnosis, meaning that there are no blood tests, X-rays, or other objective assessments which can confirm this condition. Physicians often use the Abnormal Involuntary Movement Scale (AIMS) to quantify movements that appear to be tardive dyskinesia. This scale grades involuntary movements on a scale of 0-4 in 10 different areas, including muscles of facial expression, lips/perioral area, jaw, tongue, upper extremities, lower extremities, neck, shoulders, hips, severity of overall movements, and patient awareness of the movements. Patients treated with antipsychotic medications should be rated before initiating treatment and every 3 months thereafter.
Healthcare professionals consider conditions such as thyroid disorders, parathyroid conditions, Sydenham chorea, syphilis, Wilson disease, and Meige syndrome (idiopathic orofacial dystonia) before making a diagnosis of tardive dyskinesia, as treatment differs for those conditions.
What are the treatment options for tardive dyskinesia?
Treatment of tardive dyskinesia is often difficult. Although discontinuation of the drug thought to be the cause of tardive dyskinesia is suggested followed by a trial of an alternate antipsychotic agent, this is not always a feasible solution for patients, and sometimes stopping the current antipsychotic medication may exacerbate the symptoms.
Is medication for tardive dyskinesia available?
- Dopamine-depleting medications, including tetrabenazine, deutetrabenazine, valbenazine, and reserpine, can alleviate symptoms of tardive dyskinesia.
- Benzodiazepines may benefit some patients.
- Botulinum toxin injections can be helpful for certain symptoms such as blepharospasm or isolated dystonia.
Are there natural remedies for tardive dyskinesia?
Some patients have successfully used Ginkgo biloba for control of their tardive dyskinesia, while vitamin E has been found to be ineffective.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
Is tardive dyskinesia reversible?
Tardive dyskinesia can be treated or even reversed in many patients. Early identification and treatment of this condition are often the most successful in controlling the symptoms.
Can tardive dyskinesia be prevented?
The most effective strategy in controlling tardive dyskinesia is prevention, which includes short-term use of antipsychotic medications and regular assessment of the need for continuing the medication. Experts recommend limiting the use of metoclopramide to less than 3 months.
What research for tardive dyskinesia is underway?
Studies looking at the potential benefit of pyridoxine and attempting to quantify the incidence of tardive dyskinesia are underway. Further information can be found at clinicaltrials.gov.
From
Brain and Nervous System Resources
- Working With Your Doctor to Manage MG
- The Struggle to Be Heard
- Myasthenia Gravis
Featured Centers
- What Are the Best PsA Treatments for You?
- Understanding Biologics
- 10 Things People With Depression Wish You Knew
American Academy of Neurology. Summary of Evidence-based Guideline for Clinicians Treatment of Tardive Syndromes.
Caroff. S. "Overcoming barriers to effective management of tardive dyskinesia." Neuropsychiatric Disease and Treatment. 2019; 15: 785-794.
Dhir, A., and T. Schilling, V. Abler, R. Potluri, and B. Carroll. "Estimation of tardive dyskinesia incidence and prevalence in the United States [abstract]." Movement Disorders. 2017; 32 (suppl 2).
Waln, O., and J. Jankovic. "An update on tardive dyskinesia: from phenomenology to treatment." Tremor and Other Hyperkinetic Movements. 12 July 2013; 1-11.
Waln, O., and J. Jankovic. "An update on tardive dyskinesia: from phenomenology to treatment." Tremor and Other Hyperkinetic Movements. 12 July 2013; 1-11.