Contents
- 1 Rheumatoid Arthritis vs. Polymyalgia Rheumatica
Rheumatoid Arthritis vs. Polymyalgia Rheumatica
Polymyalgia rheumatica (PMR) and rheumatoid arthritis (RA) are similar diseases.
The names RA and PMR sound similar, and that is not a coincidence.
- Both are autoimmune illnesses where the immune system attacks connective tissues, causing joint pain and stiffness.
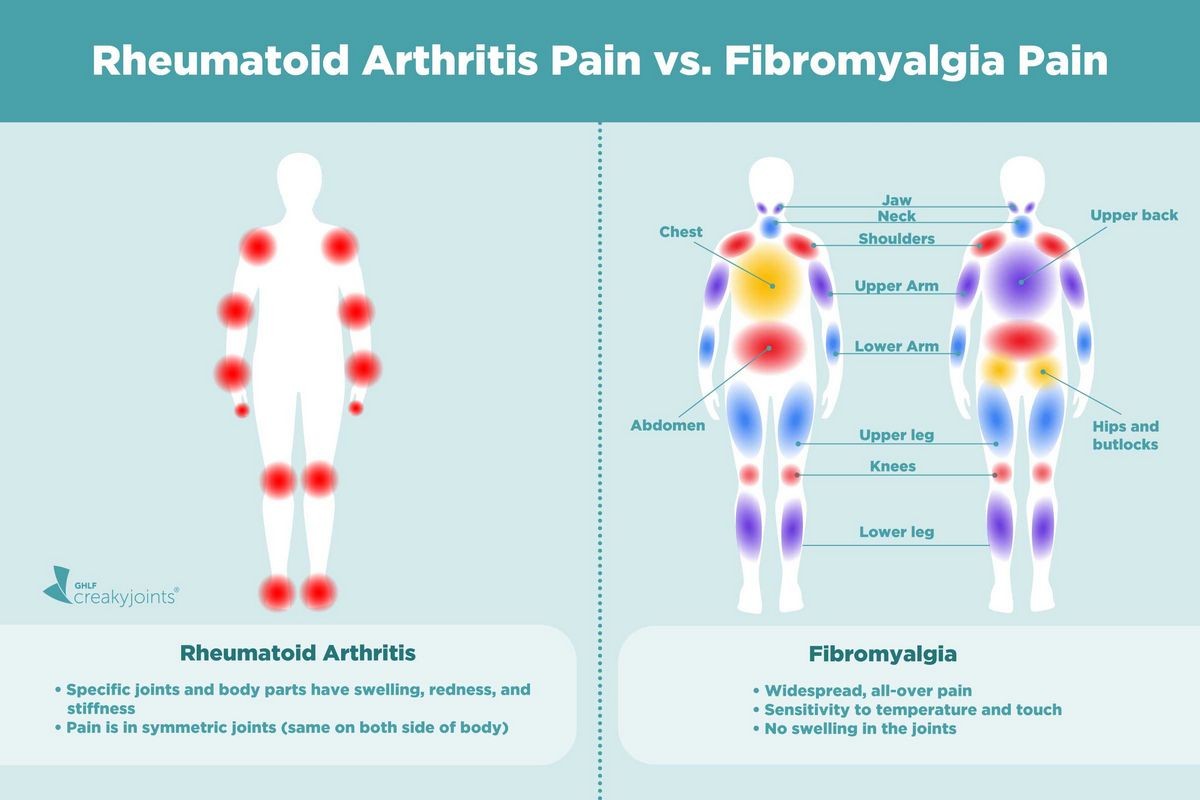
- However, swelling is only present in RA, which is a major difference.
Identifying these autoimmune disorders is challenging because their symptoms resemble those of other inflammatory and autoimmune diseases. They can cause a wide range of symptoms, and an individual may only experience a few that are not typical of the disease.
Differences between RA and PMR
- Pain, swelling, and stiffness are symptoms of chronic inflammation.
- RA can lead to bone and joint deterioration over time, resulting in disability.
- The most commonly affected areas are the wrists, fingers, knees, feet and ankles, and elbows.
- Other symptoms include:
- Tiredness and lack of energy
- Fever
- Sweating
- Poor appetite
- Weight loss
- PMR is characterized by sudden severe pain and stiffness in the shoulders, neck, hip, and lumbar spine.
- The pain usually worsens in the morning and can last for several hours.
- Other symptoms include:
- Fatigue
- Fever
- Weight loss
- Depression
QUESTION
8 common causes and risk factors of rheumatoid arthritis
Rheumatoid arthritis (RA) is an inflammatory disease that affects the body’s joints, causing severe swelling of the joint lining. Although the exact cause of RA is unknown, various factors can increase the risk of developing the disease.
- Genetic factors:
- A person is more likely to develop RA if their close family members have the disease.
- However, genetic factors alone cannot predict the disease but can increase the risk if other triggers are present.
- Hormones: Women are more likely than men to get RA, suggesting that hormones play a role in its development.
- Estrogen
- Testosterone
- Menopause
- Age: RA can develop at any age, but the risk increases with age and is more common in people in their 60s, according to the CDC.
- Smoking:
- Smokers have a higher risk of developing RA compared to nonsmokers. Smoking can modify the body’s immune response, especially in genetically predisposed individuals.
- Exposure to certain triggers, such as cigarette smoking during childhood, can increase the risk of developing RA later in life.
- Stress:
- Chronic stress can worsen RA symptoms because it is a pro-inflammatory state.
- Many individuals with rheumatic diseases report experiencing stressful events before the onset of symptoms.
- Obesity:
- Obesity is associated with an increased risk of developing RA.
- Obesity can exacerbate the adverse effects of RA by inducing metabolic disorders and cellular inflammation, according to research.
- Cellular inflammation is a common factor in both obesity and metabolic disorders.
- Past Infection: A previous infection can trigger RA by affecting the immune system’s response to specific organisms and causing an overreaction that leads to the production of new antigens.
- Diet: Certain dietary items may trigger the onset of RA, according to researchers.
While some factors are unavoidable, quitting smoking, maintaining a healthy weight, and following a diet low in processed foods may help manage RA symptoms for some individuals.
Drugs That SlowRA’s Progress
6 common causes and risk factors of polymyalgia rheumatica
Polymyalgia rheumatica (PMR) is a condition characterized by significant pain and stiffness in large muscle groups throughout the body. The exact cause of PMR is unknown, but scientific evidence suggests that it may result from the interaction of various factors.
- Genetic predisposition: There is evidence to suggest that hereditary factors may increase the susceptibility to PMR.
- Viral Infections:
- PMR has been associated with seasonal viral infections. The cyclic pattern of symptom onset and occasional remission in PMR patients can be explained by the replication patterns of viruses.
- Notably, adenovirus, human parainfluenza virus, and parvovirus B19 have been linked to PMR.
- Age:
- PMR affects only adults aged 60 years and older.
- The aging process is sometimes implicated as a cause.
- Ethnicity:
- PMR is more commonly observed in Caucasians, although it can affect individuals of all ethnicities.
- People of Northern European and Scandinavian descent have the highest risk of developing the disease.
- Gender: PMR occurs in both males and females, but it is more frequently seen in women.
- Others:
- In rare cases, PMR can occur alongside cancer.
- Overexposure to ultraviolet radiation from the sun, which damages the superficial arteries, is another hypothesized cause of PMR.
- According to some studies, ultraviolet rays can harm the elastic fibers in arteries and synovial membranes. These damaged tissues may become infected by dormant viruses that reactivate, leading to PMR.
New cases of polymyalgia rheumatica tend to appear in cycles, suggesting the involvement of environmental triggers, such as viruses.
Researchers are actively investigating the cause of PMR. The disease can develop rapidly and is more prevalent during specific seasons of the year.
What are the treatment options for PMR and RA?
Polymyalgia rheumatica
Early treatment is usually recommended for polymyalgia rheumatica (PMR). Most PMR patients are prescribed anti-inflammatory medications.
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- NSAIDs help relieve the pain and inflammation associated with PMR.
- They are not as effective as prednisone in the initial treatment of PMR but can be useful when combined with prednisone.
Rheumatoid arthritis
There is no known cure for RA. The goal of treatment is often to reduce pain and flares, minimize inflammation, and preserve joint function. Patients may receive one or more types of treatment.
- Low-dose steroids and disease-modifying antirheumatic drugs (DMARDs) offer effective management.
- Steroid injections and biologic DMARDs suppress the immune system component responsible for RA.
- These injectable medications can slow the progression of RA, but they may have significant side effects.
- Lifestyle changes, combined with these drugs, can help limit the progression of the disease. Physical activity is a crucial part of the healing process.
- Cognitive behavioral therapy can help patients identify pain triggers and provide coping methods to improve overall quality of life.
- Pain relievers, muscle relaxants, and low-dose antidepressants are sometimes used in combination.
- In addition to other pain management options, joint replacement solutions may be prescribed to restore mobility and reduce the need for multiple pain medications. An orthopedic surgeon can assess the potential for joint replacement.
- Joint fusion (arthrodesis) and tendon repair are common procedures.
Physical or occupational therapy may also be part of the treatment plan for RA and PMR to help maintain joint flexibility and muscle strength.
With appropriate treatment, these diseases can often be effectively and quickly managed, allowing individuals to continue their daily activities.
Subscribe to MedicineNet’s Arthritis Newsletter
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also understand that I may opt out of MedicineNet subscriptions at any time.