Contents
- 1 Pulmonary Edema
- 1.0.1 What causes pulmonary edema?
- 1.0.2 What are risk factors for pulmonary edema?
- 1.0.3 What are the symptoms of pulmonary edema?
- 1.0.4 When should I seek medical care for pulmonary edema?
- 1.0.5 How is pulmonary edema diagnosed?
- 1.0.6 What is the treatment for pulmonary edema?
- 1.0.7 What are the complications of pulmonary edema?
- 1.0.8 Is it possible to prevent pulmonary edema?
- 1.0.9 Subscribe to MedicineNet’s Allergy and Asthma Newsletter
Pulmonary Edema
Edema refers to swelling. It occurs when fluid seeps outside blood vessels into surrounding tissues due to:
- Excessive pressure in blood vessels
- Insufficient proteins in the bloodstream to retain fluid in the plasma
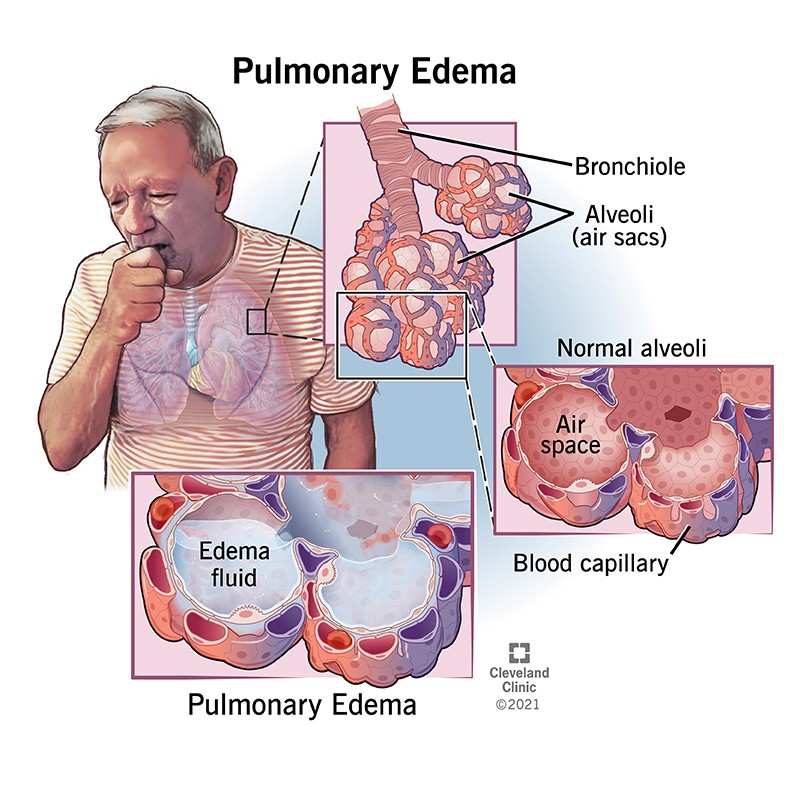
Pulmonary edema occurs when swelling happens in the lungs. The immediate area outside the small blood vessels in the lungs contains tiny air sacs called alveoli. Oxygen from the air is picked up by the blood passing through the alveoli, while carbon dioxide from the blood is released into the alveoli to be exhaled. Normally, fluids are kept out of the alveoli by their thin walls, which allow for gas exchange.
Pulmonary edema occurs when excess fluid seeps into the alveoli instead of air. This compromises gas exchange, leading to difficulty breathing and inadequate oxygenation of blood. It is often described as "water in the lungs".
Pulmonary edema can be caused by various factors. It may be related to heart failure, known as cardiogenic pulmonary edema, or have other causes called non-cardiogenic pulmonary edema.
What causes pulmonary edema?
Pulmonary edema can be caused by cardiogenic and non-cardiogenic factors. Common causes include:
Cardiogenic causes of pulmonary edema
Cardiogenic pulmonary edema is caused by high pressure in the lungs’ blood vessels due to poor heart function. This can occur due to:
- Congestive heart failure resulting from various causes such as arrhythmias, heart muscle diseases, or heart attacks
- Abnormal heart valves
High pressure forces fluid out of the blood vessels into the alveoli.
Non-cardiogenic causes of pulmonary edema
Non-cardiogenic pulmonary edema can be caused by:
- Acute respiratory distress syndrome (ARDS), a potentially serious condition caused by severe infections, trauma, lung injury, inhalation of toxins, lung infections, smoking, or radiation. In ARDS, the alveoli’s integrity is compromised, leading to fluid accumulation.
- Kidney failure and the inability to remove fluid from the body, resulting in fluid buildup in blood vessels and pulmonary edema. Dialysis may be required for advanced kidney disease.
- High-altitude pulmonary edema occurring with rapid ascent above 10,000 feet.
- Brain injuries such as brain trauma, bleeding in the brain, severe seizures, or brain surgery, leading to fluid accumulation in the lungs (neurogenic pulmonary edema).
- Lung problems causing rapid expansion and re-expansion pulmonary edema. This may occur when a collapsed lung (pneumothorax) is reinflated or when a large amount of fluid around the lung (pleural effusion) is drained.
- Overdose of heroin or methadone, or chronic high-dose aspirin use, leading to aspirin intoxication, particularly in the elderly.
- Rare causes such as pulmonary embolism, transfusion-related acute lung injury (TRALI), certain viral infections, or eclampsia in pregnant women.
IMAGES
What are risk factors for pulmonary edema?
Risk factors for pulmonary edema are essentially the underlying causes of the condition. Specific risk factors for pulmonary edema, other than the causative conditions, are not well-defined.
What are the symptoms of pulmonary edema?
The most common symptom is shortness of breath. It may occur gradually or have a sudden onset in acute cases.
Other common symptoms may include fatigue, dyspnea on exertion (shortness of breath with usual activity), rapid breathing, dizziness, and weakness. Low blood oxygen levels and abnormal lung sounds (rales or crackles) may also be detected upon examination.
When should I seek medical care for pulmonary edema?
Medical attention should be sought for diagnosed cases of pulmonary edema, which often require hospitalization. Follow-up visits may be recommended for chronic cases, such as congestive heart failure.
Treatment for pulmonary edema is typically performed by internal medicine doctors, heart specialists, or pulmonary specialists.
How is pulmonary edema diagnosed?
Chest X-ray
Pulmonary edema is typically diagnosed through chest X-rays, which show increased whiteness over the lung fields due to fluid-filled alveoli.
Medical history and physical exam
Assessing the patient’s medical history and performing a physical examination help identify the cause of pulmonary edema.
Measurement of protein markers
B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements can help determine whether cardiac or non-cardiac factors are involved. Elevated BNP levels suggest cardiac pulmonary edema, while values below 100 essentially rule out heart failure.
Swan-Ganz catheter
In critical situations, a pulmonary artery catheter (Swan-Ganz) may be used to directly measure the pressure in pulmonary vessels. A wedge pressure of 18 mmHg or higher indicates cardiogenic causes, while a lower pressure favors non-cardiogenic causes. This procedure is typically performed in the intensive care unit.
What is the treatment for pulmonary edema?
Treatment depends on the cause and severity of pulmonary edema:
- Cardiac pulmonary edema is often treated with diuretics and other heart failure medications. Severe cases may require hospitalization and intravenous diuretics.
- Treatment for non-cardiac cases varies based on the cause. Examples include antibiotics for severe infection and appropriate management for kidney failure.
- Oxygen supplementation is necessary if blood oxygen levels are low. Mechanical ventilation may be required for serious conditions like ARDS.
What are the complications of pulmonary edema?
Complications arise from the underlying causes and poor oxygenation of the blood. Diminished oxygen delivery can affect various organs, including the brain.
Is it possible to prevent pulmonary edema?
Preventive measures depend on the cause. Long-term prevention of heart disease, heart attacks, slow elevation to high altitudes, and avoidance of drug overdose are possible preventive strategies. However, some causes may not be completely avoidable, such as ARDS due to infections or trauma.
Subscribe to MedicineNet’s Allergy and Asthma Newsletter
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and understand that I may opt out of MedicineNet subscriptions at any time.


