Contents
- 1 Pheochromocytoma
- 1.0.1 What is a pheochromocytoma?
- 1.0.2 What are the stages of pheochromocytoma?
- 1.0.3 How do you know if you have pheochromocytoma?
- 1.0.4 What can be mistaken for pheochromocytomas?
- 1.0.5 What are the possible causes of pheochromocytoma?
- 1.0.6 What is the best test for diagnosing pheochromocytoma?
- 1.0.7 Is pheochromocytoma curable?
- 1.0.8 Is pheochromocytoma fatal?
Pheochromocytoma
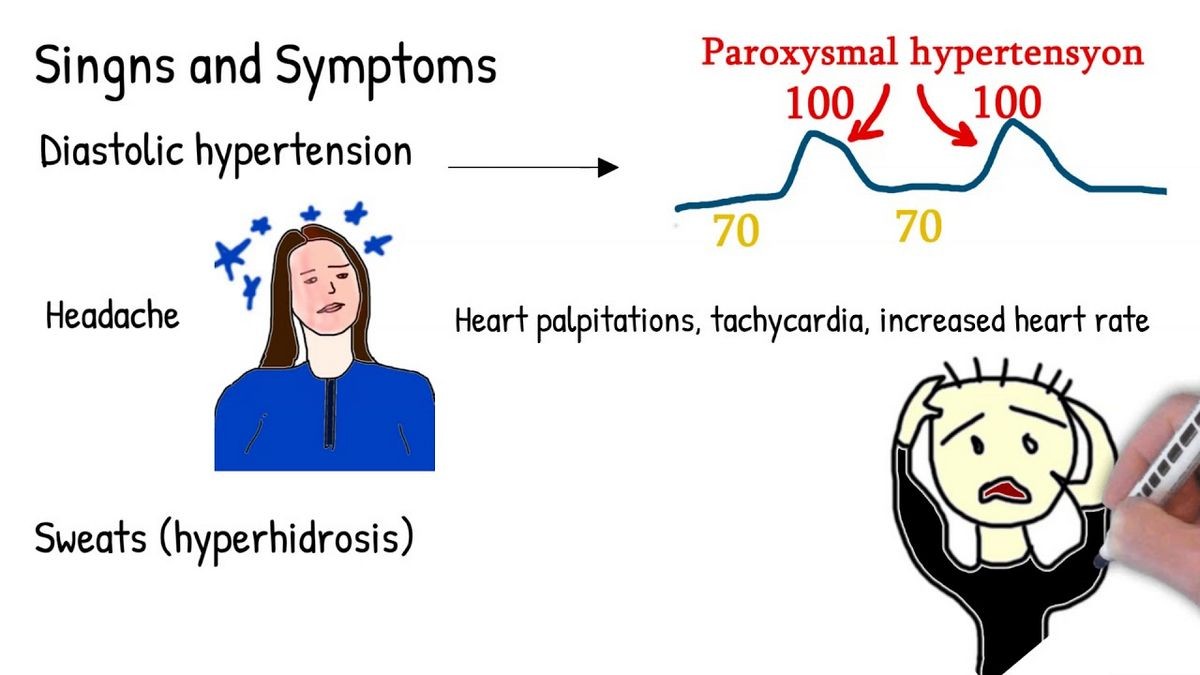
Someone with pheochromocytoma typically experiences three key symptoms: headache, sweating, and heart palpitations (fast heartbeat) alongside significantly elevated blood pressure (hypertension).
- Pheochromocytoma is a rare tumor of the adrenal glands or specialized cells outside of the adrenal glands.
- Headache, sweating, and a fast heartbeat are typical symptoms, often accompanied by high blood pressure. A pheochromocytoma releases catecholamine hormones (adrenaline and related hormones) which cause these characteristic symptoms.
- About 10% of pheochromocytomas are malignant.
- The treatment of choice is surgery.
- Pheochromocytomas can occur alongside other tumors, conditions, and in certain inherited syndromes.
What is a pheochromocytoma?
Pheochromocytomas are adrenal gland tumors that can release high levels of epinephrine and norepinephrine. The adrenal glands, located near the kidneys, are responsible for various endocrine functions. Different regions in these glands have distinct endocrine functions. The outer portion, called the adrenal cortex, secretes cortisol and aldosterone. The inner area, known as the adrenal medulla, secretes catecholamines—epinephrine, norepinephrine, and dopamine. Pheochromocytomas are tumors of these catecholamine-secreting cells, causing the symptoms discussed below. This type of cell is also found in other parts of the body.
Pheochromocytomas may also arise from chromaffin cells located outside of the adrenal gland, known as extra-adrenal pheochromocytomas or paragangliomas, usually found in the abdomen.
Pheochromocytomas can occur at any age, with the highest incidence between the third and fifth decades of life. Although rare, most cases are benign.
What are the stages of pheochromocytoma?
Pheochromocytomas are not typically staged like other cancers. The following classifications describe pheochromocytomas:
- Non-secreting pheochromocytoma: Tumors that do not produce excess hormones and may not cause noticeable symptoms.
- Secreting pheochromocytoma: Tumors that produce excessive hormones leading to symptoms like sweating, anxiety, and high blood pressure.
- Malignant pheochromocytoma: Tumors that have spread to other parts of the body, such as the lungs, bones, or liver.
- Metastatic pheochromocytoma: Tumors that have spread to other parts of the body but may not be malignant.
How do you know if you have pheochromocytoma?
Patients with pheochromocytoma usually experience three classic symptoms: headache, sweating, and heart palpitations, coupled with significantly elevated blood pressure. Other accompanying conditions may include anxiety, nausea, tremors, weakness, abdominal pain, and weight loss.
However, some individuals never develop symptoms. Up to 10% of cases are discovered incidentally during diagnostic studies for other conditions. In some cases, high blood pressure may be intermittent and difficult to document, while in others, it remains consistently elevated and easily recorded.
Pheochromocytomas are present in only about 0.2% of people with high blood pressure. However, certain conditions may increase the likelihood of a pheochromocytoma diagnosis, as discussed below.
What can be mistaken for pheochromocytomas?
Pheochromocytomas can be associated with familial or genetic syndromes, such as multiple endocrine neoplasias (MEN), specifically MEN 2A and 2B. Individuals with MEN 2A have an increased risk of parathyroid tumors and medullary carcinoma of the thyroid. Von Hippel-Lindau syndrome and neurofibromatosis type 1 are genetic disorders linked to pheochromocytomas and other tumors.
Some cases of pheochromocytomas have no known family history. If patients have bilateral disease (pheochromocytomas in both adrenal glands) or are diagnosed before the age of 21, genetic screening is recommended.
QUESTION
What are the possible causes of pheochromocytoma?
Anything that can stimulate the sympathetic nervous system, responsible for the "fight or flight" response, may be considered a potential cause of pheochromocytoma. Examples include drug use (including excessive decongestant use), drug withdrawal, panic attacks, and spinal cord injuries, among other conditions.
What is the best test for diagnosing pheochromocytoma?
If a patient exhibits the classic symptom trio of headache, sweating, and heart palpitations, and especially if they have high blood pressure, pheochromocytoma becomes a possibility. Suspicion tends to increase when young patients have no other risk factors or habits contributing to these findings.
If patients have knowledge of their family’s medical history, they can inform their doctor about other endocrine tumors, including pheochromocytomas, diagnosed in relatives. In such cases, the doctor may opt for genetic testing. Otherwise, if suspicion is high, a series of tests measuring hormones and their metabolites may be conducted:
Measurement of catecholamines and metanephrines in a 24-hour urine collection, along with possible blood tests. Levels exceeding twice the normal value usually prompt imaging tests to assess the adrenal glands. MRI or CT scans identify masses in the glands or elsewhere. If it is still unclear whether the mass is functional and relevant clinically or if imaging does not reveal a mass, a 131-I-MIBG scan can be performed. This test uses a radioactive iodine molecule to visualize pheochromocytomas in imaging studies.
Is pheochromocytoma curable?
Surgery is the definitive treatment for pheochromocytoma. Blood pressure control is crucial before and during surgery, which can be the most challenging aspect of treatment. The administration of special medications and careful monitoring of blood pressure are necessary throughout the procedure. Consultation with an endocrinologist is recommended to design appropriate treatment for individual patients.
Given the hormones involved in pheochromocytoma, blood pressure control commonly begins with alpha-blockers before considering beta-blockers to manage blood pressure response to anesthesia.
In rare cases where surgery fails to cure malignant pheochromocytomas, chemotherapy or radiation therapy may be required. Trials of targeted drugs called tyrosine kinase inhibitors have shown promise in treating pheochromocytoma and are currently being studied. Although these drug therapies cannot offer a cure, they can alleviate symptoms and sometimes prolong life.
Is pheochromocytoma fatal?
Most pheochromocytomas are benign, and with the right control of blood pressure-related complications, the prognosis is excellent. However, both malignant and benign pheochromocytomas may recur after surgery, with recurrence rates averaging around 10%. Therefore, long-term follow-up care is crucial to maintain a fair to good prognosis and administer additional appropriate treatments such as medication or surgery.
In the rare case of metastatic pheochromocytoma, survival can still be prolonged, as the disease progresses slowly. It is highly encouraged to participate in clinical trials of new therapies if metastasis is detected. When diagnosed during pregnancy, pheochromocytoma increases the mortality risk for both the mother and the fetus. It is recommended to seek immediate referral to an experienced major center in this situation.
Medically reviewed by John A. Seibel, MD, Board Certified Internal Medicine, subspecialty in Endocrinology & Metabolism


