Contents
- 1 Peritonitis
- 1.0.1 What is the most common type of peritonitis?
- 1.0.2 How does someone get peritonitis?
- 1.0.3 What are the symptoms of peritonitis?
- 1.0.4 What types of doctors diagnose and treat peritonitis?
- 1.0.5 Can a blood test detect peritonitis?
- 1.0.6 What are the three stages of peritonitis?
- 1.0.7 Is peritonitis difficult to treat?
- 1.0.8 Can peritonitis be fatal?
- 1.0.9 From
Peritonitis
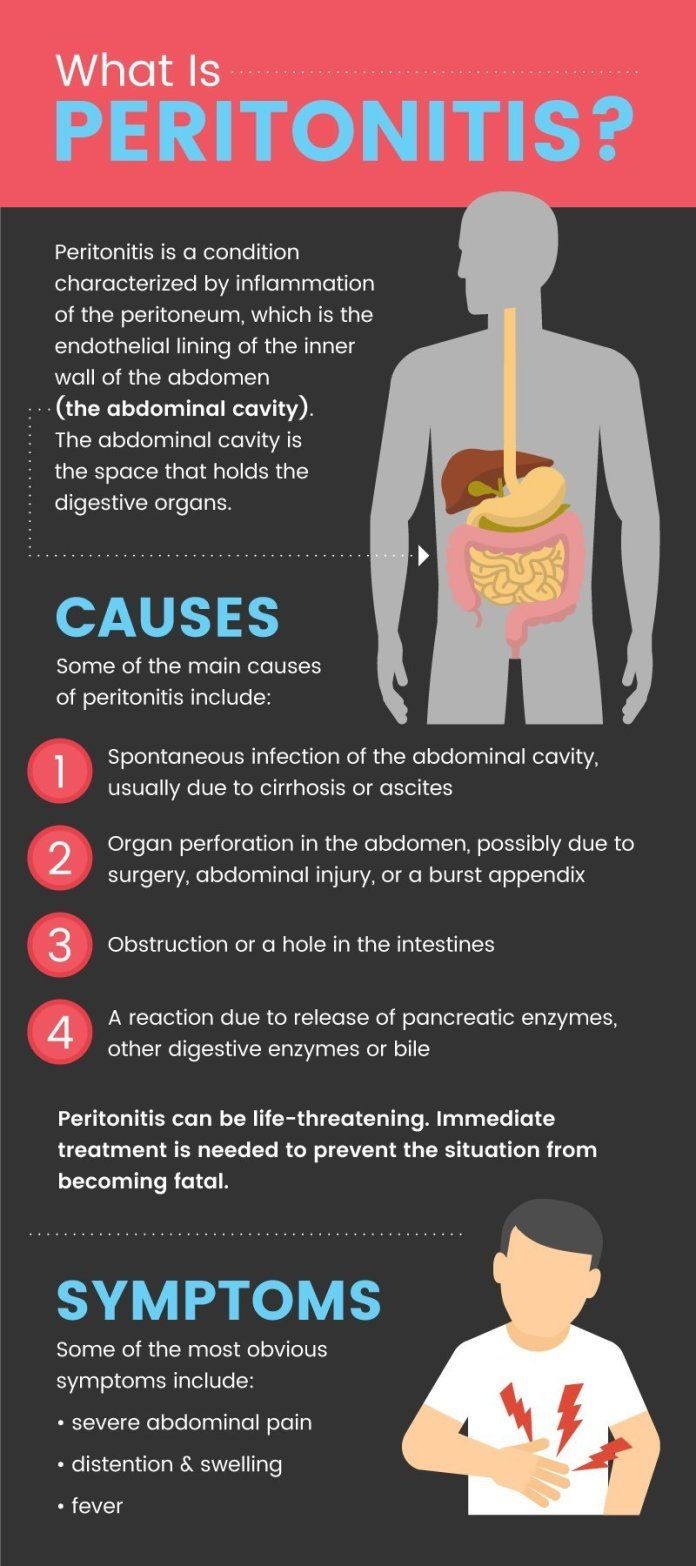
The definition of peritonitis is inflammation of the peritoneum, the thin tissue that covers the inside of the abdomen and organs within it. Peritonitis usually develops from a bacterial or fungal infection, but there are other less common causes of peritoneal inflammation.
Most individuals need quick treatment of peritonitis because infecting organisms can spread rapidly and become life-threatening.
What is the most common type of peritonitis?
The most common type of peritonitis is secondary peritonitis, usually caused by leakage or perforation of an abdominal organ, like the appendix. However, another common type of peritonitis is spontaneous bacterial peritonitis (SBP) which is most often associated with individuals that have abdominal ascites fluid.
How does someone get peritonitis?
The causes of peritonitis can be grouped into five categories.
The following is a list of these five categories and some examples of their causes:
- Primary peritonitis: Spontaneous bacterial peritonitis (SBP) is associated with ascites from patients with cirrhosis, heart failure, or systemic lupus and nephrosis. The majority of cases are caused by a microbial infection.
- Secondary peritonitis: Caused by infection due to a perforated appendix, perforated ulcers, diverticulitis, or bowel strangulation.
- Tertiary peritonitis: Caused by the bacterium Mycobacterium tuberculosis, also known as tuberculosis peritonitis.
- Chemical peritonitis: Caused by leakage of sterile fluids that are irritants to the peritoneum, such as bile, blood, or contrast agents used during procedures and tests.
- Peritoneal abscess: Caused by an infected fluid collection adjacent to visceral organs and/or the peritoneum.
Some healthcare professionals simply use a modifier placed in front of or behind the term "peritonitis" to describe the patient’s disease. Below are definitions of a sampling of some of these terms:
- Bacterial peritonitis: Any type of peritonitis caused by a bacterial species.
- Peritonitis appendicitis: Peritonitis caused by leakage of intestinal contents from the appendix.
- Acute peritonitis: Initial rapid onset of peritonitis symptoms.
- Meconium peritonitis: Sterile peritonitis caused by fetal stool escaping from the bowel before birth.
- Bile peritonitis: Leakage of bile fluid into the peritoneum.
- Septic peritonitis: Infection of the peritoneum that has spread to the blood.
- Sclerosing peritonitis: Inflammation of the abdominal cavity characterized by fibrous thickening of the peritoneum.
- Pelvic peritonitis: Inflammation involving the peritoneum surrounding the uterus and Fallopian tubes.
- Tuberculosis peritonitis: Inflammation of the peritoneum caused by Mycobacterium bacteria.
- Ascites peritonitis: Infection of ascites fluid causing inflammation of the peritoneum.
What are the symptoms of peritonitis?
People usually have abdominal discomfort and one or more of the following symptoms:
- Abdominal tenderness or pain
- Abdominal swelling
- Fever
- Chills
- Nausea
- Vomiting
- Diarrhea
- Decreased urination
- Loss of appetite
- Fatigue and/or weakness
- Constipation
- Inability to pass gas
- Ascites (fluid in the abdominal cavity)
- Unexplained encephalopathy (new-onset mental changes)
What types of doctors diagnose and treat peritonitis?
Peritonitis can rapidly develop into a life-threatening problem. Depending on its cause, different doctors will be involved in the treatment. Peritonitis is seen and treated by emergency medicine doctors, critical-care specialists, dialysis specialists, infectious disease specialists, gastroenterologists, hospitalists, internal medicine specialists, and surgeons. Other specialists may need to treat underlying causes.
Can a blood test detect peritonitis?
Early diagnosis of peritonitis is important because it can be life-threatening. Healthcare professionals will take a history and perform a physical exam on the patient. They may also order tests such as a complete cell count (CBC), blood cultures, and imaging tests like an ultrasound or CT scan of the abdomen and pelvis. In some cases, examination of dialysis fluid or abscess fluid may be necessary.
What are the three stages of peritonitis?
Peritonitis is classified into three stages based on the progression and severity of the condition:
- Acute peritonitis: The initial stage characterized by a sudden onset of symptoms including abdominal pain, tenderness, swelling, fever, nausea, vomiting, and difficulty having a bowel movement. Treatment includes antibiotics and hospitalization.
- Peritoneal abscess: Acute peritonitis can develop into a peritoneal abscess characterized by pus accumulation in the abdominal cavity. Symptoms include fever, chills, and increased abdominal pain. Treatment includes drainage of the abscess and antibiotics.
- Diffuse peritonitis: The infection spreads and causes widespread inflammation, damage to the peritoneum, and surrounding organs. Symptoms include severe abdominal pain, fever, vomiting, and signs of sepsis. Treatment includes surgery, antibiotics, and supportive care.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
Is peritonitis difficult to treat?
The treatment for peritonitis involves correcting the underlying process and administering antibiotics. Supportive care, such as avoiding dehydration and pulmonary infections, may also be necessary. In some cases, surgery is required to identify and treat the underlying cause. Antimicrobial therapy should be individualized based on the infecting organisms and their sensitivity.
Can peritonitis be fatal?
The prognosis for individuals with peritonitis depends on the underlying cause and how rapidly the disease is treated. The prognosis can range from good to poor. Prompt treatment with antibiotics and surgery often leads to a good outcome, but individuals with long-standing diseases like liver failure have a poorer prognosis.
From
Digestive Disorders Resources
- 7 Best Vitamins for Crohn’s Disease
- Side Effects From aHUS Treatment