Contents
- 1 Pancreatitis (Acute and Chronic)
- 1.0.1 Types of pancreatitis
- 1.0.2 Causes of pancreatitis
- 1.0.3 Risk factors for pancreatitis
- 1.0.4 Symptoms of pancreatitis
- 1.0.5 When to seek medical attention for pancreatitis
- 1.0.6 Diagnosing pancreatitis
- 1.0.7 Treatment of pancreatitis
- 1.0.8 Diet for pancreatitis
- 1.0.9 Prognosis and complications of pancreatitis
- 1.0.10 Preventing pancreatitis
Pancreatitis (Acute and Chronic)
Pancreatitis is inflammation of the pancreas, an abdominal gland behind the stomach in the upper abdomen. The pancreas secretes hormones and enzymes for digestion and blood sugar regulation. Digestive enzymes are activated in the small intestine to break down fats and proteins. The pancreas also releases insulin and glucagon into the bloodstream to regulate blood sugar levels.
Types of pancreatitis
Pancreatitis is categorized as acute or chronic:
- Acute pancreatitis develops suddenly and typically resolves with medical management.
- Chronic pancreatitis develops after multiple episodes of acute pancreatitis and can last for months or even years.
Pancreatitis can be mild, self-limiting, or severe and life-threatening. The most severe form can damage other organs, like the lungs and kidneys.
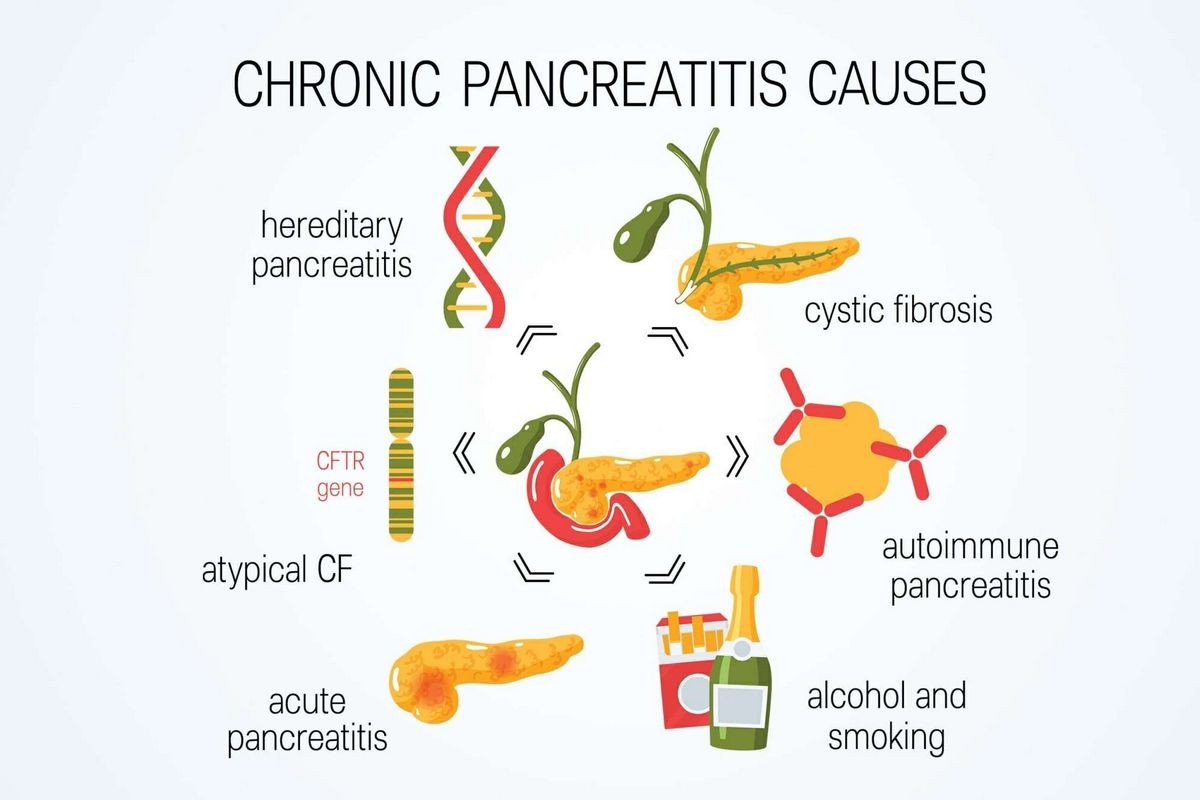
Causes of pancreatitis
Pancreatitis occurs when digestive enzymes are activated in the pancreas instead of the small intestine, leading to inflammation and damage. Causes include alcohol consumption, gallstones, high triglyceride levels, abdominal injury or surgery, certain medications, exposure to certain chemicals, smoking, family history, cystic fibrosis, and pancreatic cancer. Alcohol consumption and gallstones account for over 80% of all cases in the U.S.
Risk factors for pancreatitis
Anyone with a history of alcohol consumption or smoking has a higher risk, but anyone can develop pancreatitis. Pancreatitis diagnosed before the age of 20 is likely chronic and may continue to impact the patient throughout life.
Symptoms of pancreatitis
Pancreatitis causes upper abdominal pain ranging from mild to severe. The pain may come on suddenly or gradually, often worsening after eating. Other symptoms of acute pancreatitis include nausea, vomiting, worsening pain after eating, tenderness in the abdomen, fever, chills, weakness, and lethargy. In chronic pancreatitis, abdominal pain may be present but typically milder, and some individuals may not have any pain at all.
IMAGES
When to seek medical attention for pancreatitis
If you experience severe abdominal pain that prevents you from finding a comfortable position or sitting still, or if you have persistent stomach pain, you should contact your doctor immediately. Acute pancreatitis can lead to complications such as kidney or organ failure, pancreatic infections, necrotizing pancreatitis, and breathing problems. Chronic pancreatitis increases the risk of diabetes, malnutrition, unintentional weight loss, fat malabsorption, and pancreatic cancer.
Diagnosing pancreatitis
Tests for pancreatitis include blood tests to measure amylase and lipase levels and other tests to assess liver/kidney function, infection, and anemia. Imaging studies like CT scans and ultrasounds may be ordered to visualize the pancreas, evaluate inflammation extent, and detect gallstones and other abnormalities. Additional testing may be necessary based on the underlying cause and severity of the pancreatitis.
Treatment of pancreatitis
Most cases of acute pancreatitis require admission to the hospital, while some cases of chronic pancreatitis can be managed on an outpatient basis. Treatment varies depending on the underlying cause but typically involves fasting to rest the pancreas, IV fluids to prevent dehydration, and intravenous pain medication. Surgical intervention may be necessary for gallstone removal or to address complications like pseudocysts. Lifestyle changes, such as alcohol abstinence, may also be recommended. Medications can help manage pain, nausea, and digestive enzyme deficiencies.
Diet for pancreatitis
For people with pancreatitis, a low-fat, nutrient-rich diet is recommended, along with adequate fluid intake to prevent dehydration.
Prognosis and complications of pancreatitis
The prognosis for pancreatitis depends on various factors, including the underlying cause, severity, age, and general health of the patient. Complications can range from a self-limited illness to severe complications like diabetes, pseudocyst formation, malnutrition, and pancreatic cancer. Infections can lead to multi-organ failure, sepsis, and death. Repeated episodes of acute pancreatitis can result in chronic pancreatitis, negatively impacting quality of life.
Preventing pancreatitis
Lifestyle changes, such as alcohol and smoking cessation, maintaining a healthy weight, and consuming a low-fat diet, can reduce the risk of pancreatitis.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
Sources:
American College of Gastroenterology: "Gallstone Pancreatitis."
Digestive Diseases and Sciences: "Complications of Chronic Pancreatitis."
Gastroenterology: "The Epidemiology of Pancreatitis and Pancreatic Cancer."
Institute for Quality and Efficiency in Health Care: "How does the pancreas work?"
Merck Manual: "Acute Pancreatitis."
National Institute of Diabetes and Digestive and Kidney Diseases: "Symptoms and Causes of Pancreatitis."
National Institute of Diabetes and Digestive and Kidney Diseases: "Treatment for Pancreatitis."
The National Pancreas Foundation: "About Chronic Pancreatitis"
The National Pancreas Foundation: "Acute Pancreatitis Testing and Diagnosis."
The National Pancreas Foundation: "Fact Sheet – Pancreatic Disease."
The National Pancreas Foundation: "Hereditary pancreatitis."
StatPearls: "Alcoholic Pancreatitis."


