Contents
- 1 Meniere’s Disease (Meniere Disease)
- 1.0.1 What causes Meniere’s disease?
- 1.0.2 What are the symptoms of Meniere’s disease?
- 1.0.3 How is Meniere’s disease diagnosed?
- 1.0.4 How can Meniere’s disease be treated?
- 1.0.5 What surgical procedures can treat Meniere’s disease?
- 1.0.6 What is the prognosis for Meniere’s disease?
- 1.0.7 What are the complications of surgery for Meniere’s disease?
Meniere’s Disease (Meniere Disease)
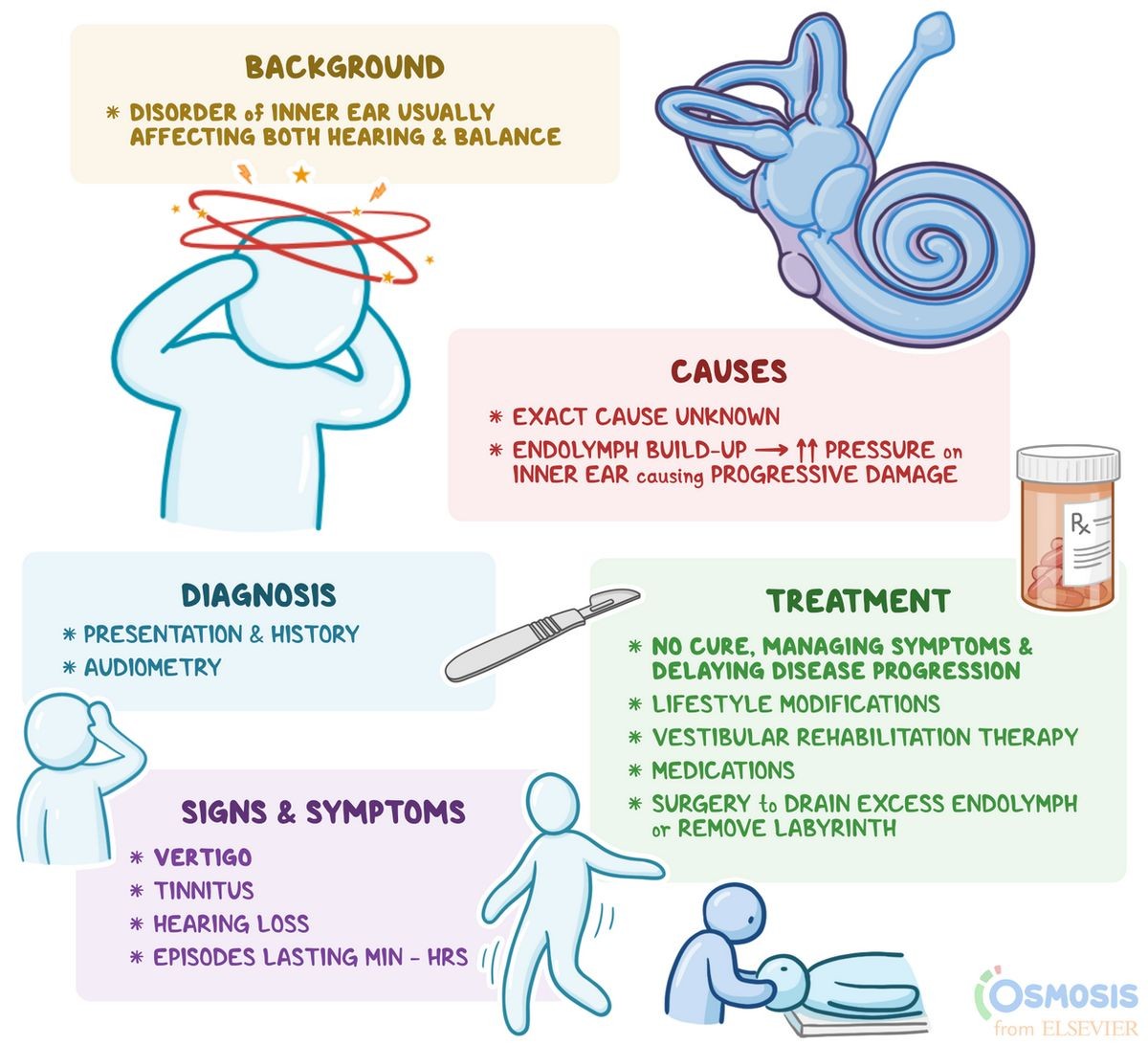
Meniere disease, an inner ear disorder, causes hearing loss, ringing, ear fullness, and poor equilibrium.
Meniere’s disease disrupts fluid flow in the inner ear, resulting in chronic symptoms such as hearing loss, vertigo, and ringing in the ears. Surgical options are available for severe or medication-resistant cases of Meniere’s disease.
What causes Meniere’s disease?
The cause of Meniere’s disease is unknown, but it likely involves abnormalities in inner ear fluid regulation.
- In most cases, only one ear is affected, but about 15% of patients have both ears involved.
- Meniere’s disease typically starts between ages 20 and 50, but it can occur in any age group.
- Men and women are equally affected by the disease.
- The symptoms may range from minor annoyance to disabling, especially if vertigo attacks are severe, frequent, and unexpected.
- Meniere’s disease is also known as idiopathic endolymphatic hydrops.
What are the symptoms of Meniere’s disease?
Meniere’s disease symptoms commonly include:
- Episodic rotational vertigo: This symptom manifests as spinning sensations accompanied by disequilibrium, nausea, and sometimes vomiting. Vertigo attacks can last from 20 minutes to several hours. Patients may experience an off-balance sensation that can persist for days.
- Tinnitus: A roaring, buzzing, machine-like, or ringing sound in the ear. Tinnitus may be episodic, appearing with vertigo attacks, or constant. It often worsens before vertigo onset.
- Hearing loss: Initially intermittent, but over time may become permanent. The loss tends to affect lower frequencies and can make loud sounds uncomfortable or distorted.
- Ear fullness: Sensation of fullness in the ear, which typically precedes vertigo attacks.
How is Meniere’s disease diagnosed?
Diagnosis of Meniere’s disease primarily relies on history and physical examination. Tinnitus or ear fullness must be present to confirm the diagnosis.
An audiogram can confirm hearing loss and rule out other abnormalities. In some cases, an audiogram during or immediately after a vertigo attack may reveal low-frequency hearing loss. As the disease progresses, hearing loss tends to worsen.
Additional tests, such as auditory brain stem response (ABR), computerized tomography (CT scan), or magnetic resonance imaging (MRI), may be necessary to rule out tumors on the hearing or balance nerve. A complete neurological evaluation is performed to rule out other vertigo causes.
QUESTION
How can Meniere’s disease be treated?
Treatment options for Meniere’s disease include:
- Medications: Diuretics, combined with a low-salt diet, are the primary treatment. Anti-vertigo medications and anti-nausea medications may be prescribed to alleviate symptoms. Steroids or antibiotic injections into the middle ear may provide relief from vertigo symptoms.
- Air pulse generator: Some patients may benefit from periodic delivery of small air pulses through a tube placed in the eardrum.
- Surgery: Surgical procedures such as endolymphatic shunt, selective vestibular neurectomy, or labyrinthectomy may be recommended if vertigo attacks are medically uncontrollable and disabling.
What surgical procedures can treat Meniere’s disease?
Prior to surgery for Meniere’s disease, doctors will carefully evaluate the patient’s general health and ability to withstand surgery and anesthesia. Contraindications for surgery include:
- Active otitis media or mastoiditis: Infections must be resolved before proceeding with surgery.
- Bilateral Meniere’s disease is often a contraindication for labyrinthectomy due to the risk of permanent imbalance.
- Poor general health.
Surgical procedures for Meniere’s disease include:
- Endolymphatic sac surgery: During this procedure, doctors remove a small amount of bone around the endolymphatic sac to reduce fluid pressure. The surgery can be performed using osseous labyrinthectomy or by destroying soft tissue in the inner ear. The procedure involves cutting nerve fibers related to balance and does not affect hearing ability.
What is the prognosis for Meniere’s disease?
Although there is no cure for Meniere’s disease, vertigo attacks can usually be managed. Patients with unpredictable vertigo should refrain from driving to ensure safety. Success rates for surgery depend on the specific procedure:
- Endolymphatic sac surgery controls vertigo in about 6 to 9 out of 10 patients. Hearing may improve over time, but there is a low risk of hearing loss.
- Labyrinthectomy and vestibular nerve sectioning have success rates of about 95-98% but carry a higher risk of hearing loss.
- Trans tympanic injection of medications is a relatively new approach with reported success rates near 90%, though its overall efficacy is still being determined.
What are the complications of surgery for Meniere’s disease?
Surgery for Meniere’s disease has potential complications, although they are rare. Specific risks depend on the type of surgery. Common complications may include:
- Hearing loss
- Tinnitus
- Dizziness
- Facial paralysis
- Hematoma
- Bleeding
- Cerebrospinal fluid leakage
- Taste disturbance
- Mouth dryness
- Ear infections
- Ear drainage
- Meningitis
- Headaches
It is normal to experience severe vertigo and imbalance for the first few days following surgery. Doctors may prescribe medication to alleviate nausea and vomiting during this period.
Moskowitz, Howard S., M.D., Ph.D. "Meniere disease." UptoDate.com. Updated Mar. 22, 2016


