Contents
How Long Can a Person Live With Hepatitis C?
Hepatitis C causes liver inflammation and its impact on lifespan depends on disease progression and timely treatment.
Hepatitis C is a condition that inflames the liver. If left untreated, it can lead to severe disorders such as liver cirrhosis, liver failure, and liver cancer, significantly reducing lifespan. Roughly 30% of people with hepatitis C will naturally clear the virus within six months of infection without treatment. The remaining 70% develop chronic hepatitis, with up to 30% progressing to liver cirrhosis. Understanding the causes, progression, diagnosis, and treatment of hepatitis C is critical to evaluating lifespan after diagnosis. The impact on lifespan depends on disease progression and the effectiveness of timely treatment.
The cause of hepatitis C is the hepatitis C virus (HCV). HCV may cause both acute and chronic infections. Acute HCV infections do not typically cause life-threatening disease and often resolve within six months without treatment. However, chronic HCV infections can lead to severe conditions like liver cirrhosis within 20 years of initial infection. HCV infection can be mistaken for other causes of liver inflammation, such as excessive alcohol consumption, certain medications, or exposure to toxic substances.
Main Symptoms of Hepatitis C
Hepatitis C often remains asymptomatic for the first two to three months after infection. Symptoms commonly associated with acute hepatitis C include:
- Fatigue
- Fever
- Joint pain
- Loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Nausea and vomiting
- Pale colored stool
- Abdominal pain
Chronic hepatitis C infections may not show symptoms until years later, which can lead to the development of liver conditions such as cirrhosis and liver cancer. Liver disorders caused by hepatitis C progress slowly and are often asymptomatic, only getting detected during blood transfusions or routine tests.
How is Hepatitis C Transmitted?
Hepatitis C spreads through contact with the body fluids of an infected person. Methods of transmission include:
- Sexual contact: Hepatitis C can spread through unprotected sexual contact, including among males who have sex with other males.
- Birth: Children born to mothers with hepatitis C are at risk of being born with the infection.
- Tattoos and body piercing: Unsterilized equipment during tattooing or body piercing can transmit hepatitis C.
- Sharing sharp objects: Sharing razors, needles, or toothbrushes with an infected person can cause transmission.
- Blood transfusions or organ transplants: Although rare now, blood transfusions or transplants with poorly screened organs or blood can transmit hepatitis C.
- Unsterilized drug injection equipment: Sharing syringes, needles, or other drug injection equipment can transmit hepatitis C.
Hepatitis C cannot be spread through hugging, kissing, holding hands, breastfeeding, coughing, or sharing food, water, and utensils. Even after successful treatment and cure, there is still a risk of reinfection, especially when sharing sharp objects with an infected person. Individuals with kidney failure on maintenance hemodialysis are at a higher risk of infection and reinfection and should consider regular testing.
Diagnosis of Hepatitis C
New infections of hepatitis C are often asymptomatic, making early diagnosis difficult. Chronic hepatitis C infections also remain asymptomatic until liver damage occurs. Diagnosis is usually done using two types of tests:
- Serological tests: These tests detect anti-HCV antibodies and identify people who have been exposed to hepatitis C.
- Nucleic acid test (NAT) for HCV RNA: NAT testing confirms the presence of the virus in people with positive serological tests. It helps identify chronic infections, as acute infections are typically cleared by the body’s immune system. Some people may test positive for anti-HCV antibodies from previous exposures even if they are not currently infected.
When chronic infections are confirmed, further testing, such as a liver biopsy or a non-invasive test, can determine the extent of liver damage (cirrhosis) for appropriate treatment and management.
Early diagnosis is crucial for successful treatment of hepatitis C. With early intervention, treatment duration can be as short as eight to twelve weeks.
QUESTION
Treatment for Hepatitis C
If recently infected with hepatitis C, treatment may not be necessary unless the infection becomes chronic since some people can naturally cure the condition through an immune response.
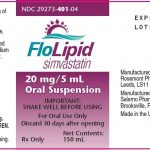
Doctors may choose to wait until the infection becomes chronic before initiating treatment. The World Health Organization (WHO) recommends starting therapy with pan-genotypic direct-acting antiviral agents (DAAs) to cure most hepatitis C infections in individuals aged 12 and older. Treatment typically lasts about 12 weeks, depending on the presence of cirrhosis.
Potential Complications of Hepatitis C
Without early diagnosis and treatment, hepatitis C can lead to the following complications:
- Liver cirrhosis: Healthy liver tissue gets replaced by scar tissue, blocking blood flow and causing liver dysfunction.
- Liver cancer: Chronic hepatitis C increases the risk of hepatocellular carcinoma (liver cancer), even after treatment. Regular tests are recommended to detect liver cancer early for better treatment options, including liver transplant if necessary.
- Liver failure: Progressive liver dysfunction over months or years can lead to end-stage liver disease.
Early diagnosis and treatment are crucial for improving lifespan. Studies suggest that approximately 20% of people with chronic hepatitis C develop liver cirrhosis within 20 years, with a further 20% developing hepatocellular carcinoma, both of which can cause premature death.
If hepatitis C causes advanced liver issues, it is important to consult with a specialist who can recommend appropriate treatment options, such as medications or surgery. In extreme cases, a liver transplant may be considered.
Impact on Lifespan
A study conducted in New York City between 2000 and 2011 showed that people with hepatitis C had an average lifespan of 60 years, compared to 78 years for those without the infection. Co-infection with HIV further reduced the average lifespan to 52 years.
While this study focused on NYC, it supported previous research indicating that people with hepatitis C face a higher risk of premature death compared to the general population, with life expectancy decreasing with age. However, with proper diagnosis, early intervention, and effective treatment, the lifespan of individuals with hepatitis C can be significantly improved. Regular follow-ups with healthcare professionals are essential for achieving the best outcome.
Sources:
Centers for Disease Control and Prevention: "Hepatitis C Questions and Answers for the Public."
Clinical Infectious Diseases: "Deaths Among People With Hepatitis C in New York City, 2000–2011."
MedlinePlus: "Hepatitis C."
National Institute of Diabetes and Digestive and Kidney Disease: "Hepatitis C."
World Health Organization: "Hepatitis C."