Contents
- 1 Heart Transplant
- 1.0.1 History of the heart transplant
- 1.0.2 Who needs a heart transplant?
- 1.0.3 What is the survival rate of a heart transplant?
- 1.0.4 What are the complications of a heart transplant?
- 1.0.5 What are the symptoms of heart transplant rejection?
- 1.0.6 How is heart transplant rejection diagnosed and monitored?
- 1.0.7 Why are heart transplants not more common?
Heart Transplant
A heart transplant is a surgery in which a diseased heart is replaced with a healthy heart from a donor. Heart transplantation is a relatively simple operation for a cardiac surgeon.
There are three types of heart transplants:
- The first operation is harvesting the heart from the donor.
- The donor is usually an unfortunate person who has suffered irreversible brain injury, called "brain death".
- Often these are patients who have had major trauma to the head, for example, in an automobile accident. The victim’s organs, other than the brain, are working well with the help of medications and other "life support" that may include a respirator or other devices.
- A team goes to the hospital of the donor to remove donated organs once brain death of the donor has been determined. The organs are transported on ice to keep them alive until they can be implanted.
- For the heart, this is optimally less than six hours. So, the organs are often flown by airplane or helicopter to the recipient’s hospital.
- Removing the damaged heart may be easy or difficult, depending on whether the recipient has had previous heart surgery (as is often the case).
- If there has been previous surgery, cutting through the scar tissue may complicate removal of the heart.
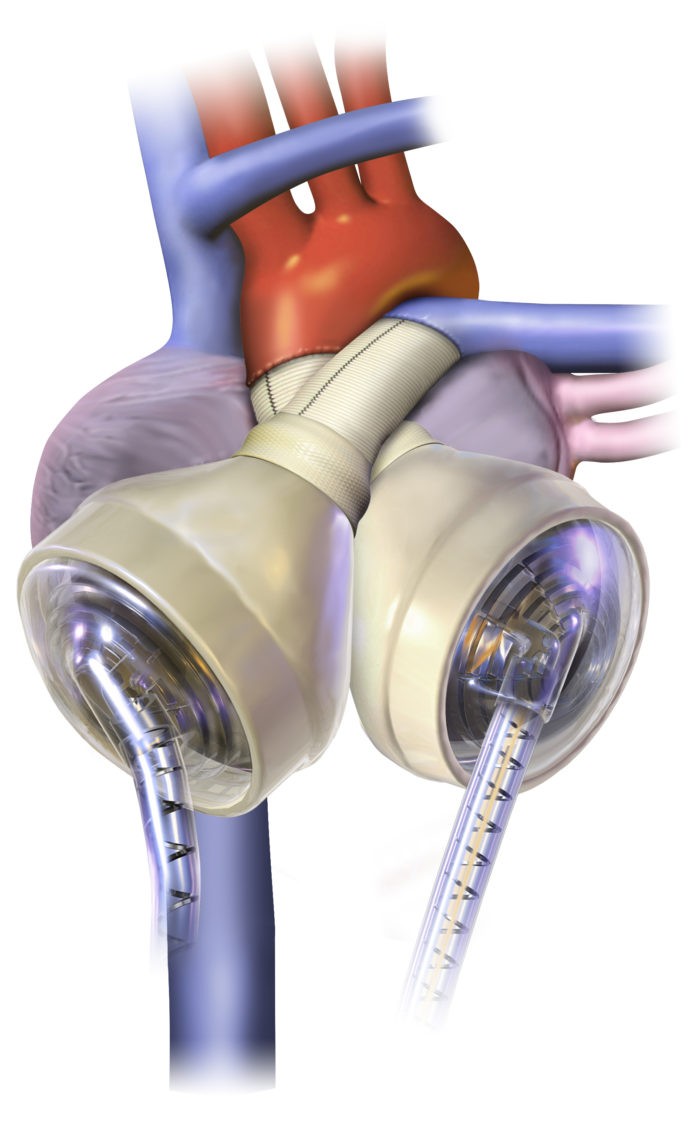
- Today, this operation involves the creation of only five lines of stitches, or "anastomoses". These suture lines connect the large blood vessels entering and leaving the heart.
- If there are no complications, most patients who have had a heart transplant are home about one week after the surgery.
- The generosity of donors and their families makes organ transplantation possible.
Picture of the Heart and Great Vessels in Heart Transplant
Picture of the Heart in the Pericardial Sac
Picture of the Interior of the Heart in the Paricardial Sac
History of the heart transplant
- The idea of replacing a bad organ with a good one has been documented in ancient mythology. The first real organ transplants were probably skin grafts that may have been done in India as early as the second century B.C.
- The first heart transplant in any animal is credited to Vladimer Demikhov. Working in Moscow in 1946, Demikhov switched the hearts between two dogs. The dogs survived the surgery.
- The first heart transplant in human beings was done in South Africa in 1967 by Dr. Christiaan Barnard; the patient only lived 18 days.
- Most of the research that led to successful heart transplantation took place in the United States at Stanford University under the leadership of Dr. Norman Shumway.
- Once Stanford started reporting better results, other centers started doing heart transplants. However, successful transplantation of a human heart was not ready for widespread clinical application until medications were developed to prevent the recipient from "rejecting" the donor heart. This happened in 1983 when the Food and Drug Administration (FDA) approved a drug called cyclosporine (Gengraf, Neoral).
- Before the advent of cyclosporine, overall results of heart transplants were not very good.
Who needs a heart transplant?
- Not everyone who needs a heart transplant can get one due to limited donor hearts. A careful selection process is in place to assure that hearts are distributed fairly and to those who will benefit most from the donor heart.
- Most patients require a transplant because their hearts can no longer pump enough blood to supply oxygen and nutrients to the organs of the body.
- A smaller number of patients have a good pump, but a bad "electrical conduction system" of the heart. This electrical system determines the rate, rhythm, and sequence of contraction of the heart muscle. Problems with the conduction system can cause sudden cardiac death.
- All the other important organs in the body must be in good shape for a heart transplant. Transplants cannot be performed in patients with active infection, cancer, or diabetes mellitus; patients who smoke or abuse alcohol are also not good candidates.
- Transplant recipients need to change their lifestyle and take numerous medications. Psychological testing is done to identify factors that could interfere with recovery, compliance with medications, and necessary lifestyle changes after transplantation.
- A suitable donor heart must be compatible with the recipient’s immune system.
- The United Network for Organ Sharing (UNOS) ensures equitable allocation of organs to individuals who will benefit the most from transplantation.
QUESTION
What is the survival rate of a heart transplant?
- When all potential problems are considered, the results of transplantation are remarkably good. Heart failure is a serious and life-threatening disease.
- In patients with severe forms of heart failure that require transplantation, the one-year mortality rate is 80%.
- After a heart transplant, five-year survival averages about 50%-60%. One-year survival averages about 85%-90%.
What are the complications of a heart transplant?
- Our body’s immune system attacks transplanted organs, causing rejection.
- Rejection can be controlled with powerful immunosuppressive medications. However, immunosuppression makes transplant patients more susceptible to infection and cancer.
- Chronic rejection, characterized by the growth of tissue that causes blockage of the heart’s blood vessels, is the major limiting factor for the long-term success of heart transplantation.
- As survival has improved, more older transplant patients are dying from cancers.
What are the symptoms of heart transplant rejection?
Rejection and infection share similar symptoms:
- weakness
- fatigue
- malaise (feeling lousy)
- fever
- "flu-like symptoms" such as chills, headaches, dizziness, diarrhea, nausea, and/or vomiting
Transplant patients with these symptoms need immediate medical attention.
Physicians will conduct tests to determine whether the transplanted heart is functioning normally or not. If there is no evidence of rejection, a thorough search for infection will be performed.
How is heart transplant rejection diagnosed and monitored?
- The gold standard for monitoring rejection is the endomyocardial biopsy, a simple operation.
- A catheter is inserted into the jugular vein and advanced into the right side of the heart to collect small samples of heart muscle for analysis.
- Less invasive methods, such as analyzing gene expression in blood samples, have been developed to decrease the frequency of biopsies.
Why are heart transplants not more common?
- Qualifying for a heart transplant is difficult. Patients must have a bad heart but a healthy body.
- The major limiting factor is the availability of donor hearts. Many individuals and families refuse to donate organs, and not all matches are suitable. Time constraints and cost are also factors.
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and I understand that I may opt out of MedicineNet subscriptions at any time.
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and I understand that I may opt out of MedicineNet subscriptions at any time.


