Contents
Excessive Sweating (Hyperhidrosis)
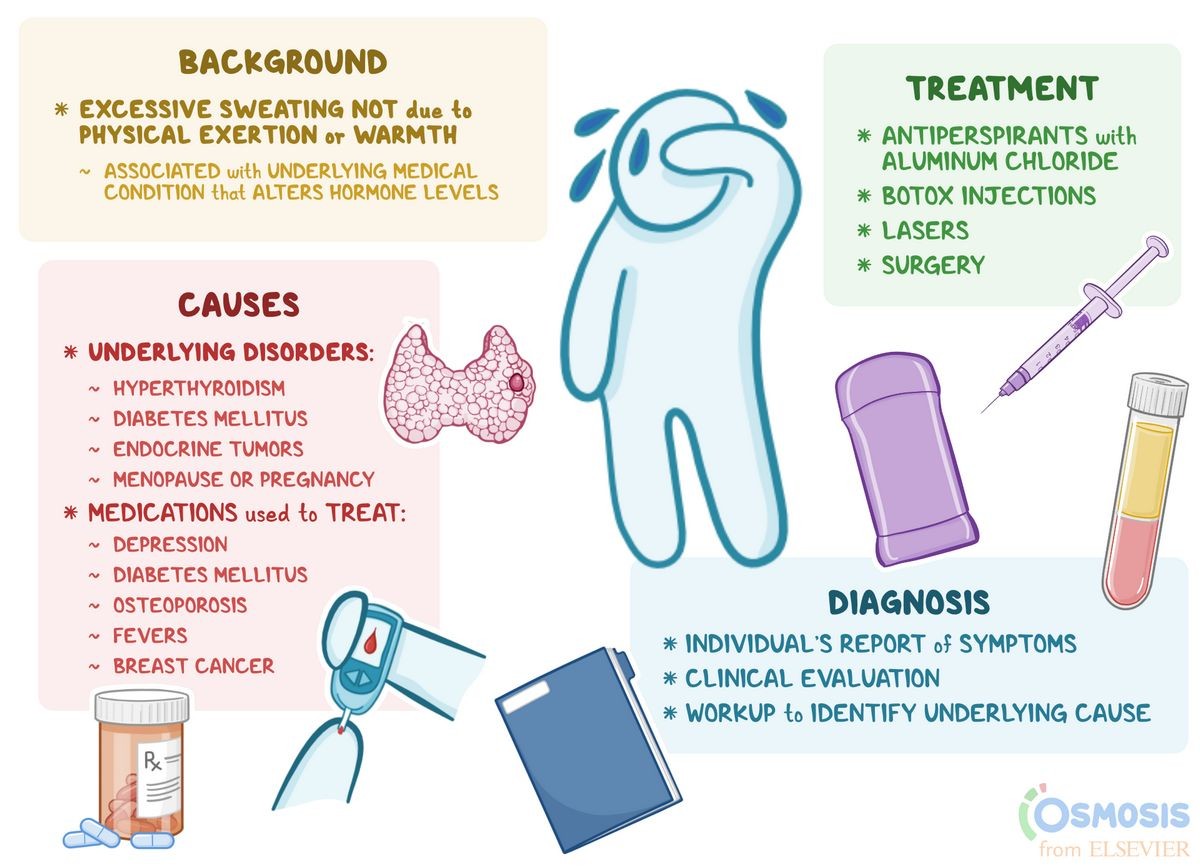
The word hidrosis is derived from the Greek and simply means "sweat." Hyperhidrosis, excessive sweat or excessive sweating, produces embarrassment and unhappiness.
- Primary hyperhidrosis occurs in healthy individuals with no apparent cause.
- Secondary hyperhidrosis is less common and can be due to drugs, systemic diseases, neurological disorders, facial surgery, and anxiety.
About 3% of Americans experience excessive sweating, with 50% affecting the underarms (axillary hyperhidrosis). Underarm problems tend to start around puberty, while palm and sole sweating may begin earlier, often during childhood. Untreated, these problems may continue throughout life.
Sweating embarrasses and stains clothes, and may complicate business and social interactions. Excessive sweat can have practical consequences, like making it difficult to hold tools, grip a steering wheel, or shake hands.
What causes hyperhidrosis excessive sweating?
Otherwise healthy people with excessive sweating have primary hyperhidrosis. Heat and emotions may trigger hyperhidrosis in some, but many who suffer from hyperhidrosis sweat nearly all the time, regardless of their mood or the weather.
Secondary hyperhidrosis can be caused by dopamine agonists, antidepressants, antipsychotics, alcohol, and insulin. Systemic disorders such as diabetes mellitus, hyperthyroidism, and Parkinson’s disease, and tumors such as pheochromocytoma and lymphoma have been associated with secondary hyperhidrosis.
What signs and symptoms accompany hyperhidrosis?
Excessive sweating is known as hyperhidrosis. Hyperhidrosis can happen to anyone who has a fever or is dealing with a bout of anxiety.
Generally, the only sign of excessive sweating is abundant moisture in the affected area. The presence of this moisture can predispose to skin infections.
What are the risk factors for hyperhidrosis?
As stated above, several conditions and diseases produce secondary hyperhidrosis. Treating the underlying condition can help relieve at least some of the excessive sweating.
How do healthcare professionals diagnose hyperhidrosis?
The diagnosis is made clinically based on a patient’s history and physical examination. If sweating is excessive and constant, then the diagnosis is obvious. Often, the patient’s history is relied upon to determine the diagnosis. Research centers measure sweat production by comparing the weight of filter paper left on the skin before and after sweating.
Dermatologists specialize in diagnosing and treating skin conditions. Dermatologists diagnose and treat this condition.
IMAGES
What are medical treatment options for hyperhidrosis?
Through a systematic evaluation of causes and triggers of excessive sweating, followed by a stepwise approach to medical treatment, many people with this disorder can achieve an improved quality of life. The decision on initial treatment depends upon the severity of the condition and the affected areas.
The approach to treating hyperhidrosis generally proceeds as follows:
- Over-the-counter antiperspirants: Patients usually try these first because they are readily available. Antiperspirants containing aluminum chloride may be more effective when others have failed. "Natural" antiperspirants are often not very helpful for patients.
- Prescription-strength antiperspirants: those containing aluminum chloride hexahydrate
- Iontophoresis: a device that uses a direct current to drive ions into the sweat gland using tap water occasionally mixed with aluminum ions or other substances
- Oral medications: from the group of medications known as anticholinergics, which reduce sweating
- Topical medicated pads: pads impregnated with anticholinergic medications for use in the armpits
- Botox (botulinum toxin): approved in the U.S. by the Food and Drug Administration (FDA) for treating excessive axillary sweating
- Microwave destruction: a device destroys the sweat glands, purportedly causing minimal damage to other tissues
- Surgery: paraspinal sympathectomy, or interruption of certain nerve pathways, as a last resort
Aluminum chloride hexahydrate
When regular antiperspirants fail, doctors often recommend aluminum chloride hexahydrate (Drysol, various generics), a prescription-strength version of aluminum chloride. It is applied just before bedtime seven to 10 nights in a row, then roughly once a week as a maintenance medication. The aluminum salts in this preparation collect in the sweat ducts of the patient and block them. Over time, the excessive perspiration may diminish to such an extent that no further treatment is needed. This method works well for many patients with underarm sweating, but it’s not satisfactory for those with clammy palms and sweating of the soles of the feet.
The main side effect of aluminum chloride is irritation, which can sometimes be overcome by reducing the frequency of use or applying anti-inflammatory medications.
Iontophoresis
Iontophoresis was introduced over 50 years ago to treat excessive sweating. Its exact mechanism of action is still unclear. The procedure uses water to conduct an electric current to the skin, which combats the production of sweat. The current is applied typically for 10-20 minutes per session, initially with two to three sessions per week followed by a maintenance program of treatments at one- to three-week intervals, depending on the patient’s response. Iontophoresis treatments sound painful but are not.
Patients purchase devices for this treatment through a doctor’s prescription. Three iontophoresis devices are registered with and cleared by the U.S. FDA; the treatment works best on palms and soles but can be adapted for use in the underarms. Medical insurers sometimes cover the cost.
Oral medicines
Oral anticholinergic drugs can be quite effective for this condition, but they can produce side effects like dry mouth, insomnia, and blurred vision. The dosage should be titrated carefully.
Topical anticholinergic pads
A new treatment using glycopyrronium tosylate-impregnated gauze pads has received approval for the treatment of armpit hyperhidrosis.
Botox
Botulinum toxin (Botox), a muscle poison used in medicine for various conditions, including excessive underarm sweating. Botox is injected into the tissues of the armpit or hand, inhibiting the release of acetylcholine, which activates sweat glands. This treatment can provide approximately six months of relief from sweating. The injections are uncomfortable, but the use of a very small needle minimizes discomfort.
Health insurers may provide coverage for Botox injections, but the treatment can be costly.
The FDA has not approved Botox for treating sweating of the palms and soles of the feet, though some physicians are administering it as an off-label use, with some success. Drawbacks of using this treatment for the palms and soles include pain and the potential for temporary muscle weakness.
Microwave, laser, and ultrasound destruction
New techniques using energy to destroy sweat glands while preserving other tissues. Currently, only the armpits seem to be appropriate treatment sites. Treatments occur in a doctor’s office and may have minor side effects like local swelling and irritation. Sweating seems to be significantly decreased for a time with these treatments. How these would be used in other areas aside from the armpits is not clear.