Contents
- 1 Claudication
- 1.0.1 What are the risk factors for claudication and peripheral vascular disease?
- 1.0.2 What causes claudication?
- 1.0.3 What are the symptoms of claudication?
- 1.0.4 What can cause the artery narrowing that leads to claudication?
- 1.0.5 Why does claudication come and go?
- 1.0.6 Who gets claudication?
- 1.0.7 How is claudication diagnosed?
- 1.0.8 What is the treatment for claudication?
- 1.0.9 Can claudication be prevented?
- 1.0.10 What is the prognosis and treatment for patients with intermittent claudication?
Claudication
Claudication is pain and cramping in the lower leg due to inadequate blood flow to the muscles. The pain usually causes the person to limp. The word "claudication" comes from the Latin word "claudicare" meaning to limp. Claudication is typically felt while walking and subsides with rest. It is commonly referred to as "intermittent" claudication because it comes and goes with exertion and rest. In severe cases, the pain is also felt at rest.
What are the risk factors for claudication and peripheral vascular disease?
Risk factors for peripheral artery disease and claudication include:
- Smoking
- Diabetes
- High blood pressure
- High cholesterol
- African American descent
- Heart disease
What causes claudication?
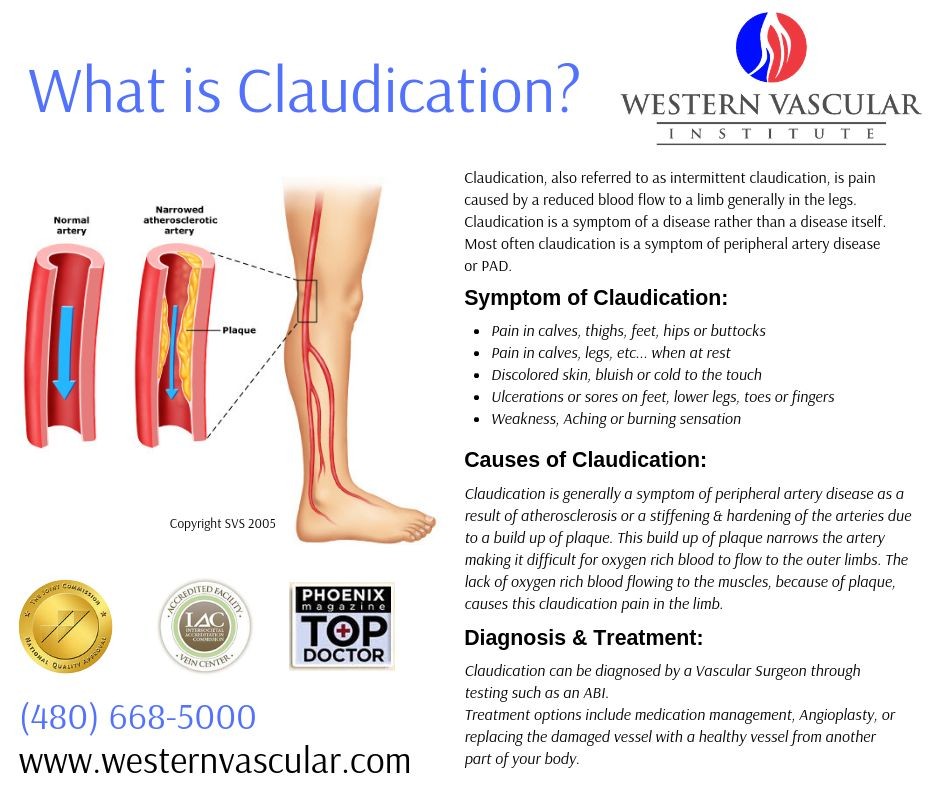
The severity of the peripheral artery disease, the location of the plaque, and the activity of the muscles determine the symptoms and the location of the pain.
Several medical problems can cause claudication, but the most common is peripheral artery disease. Peripheral artery disease (PAD) is caused by atherosclerosis, which is a hardening of the arteries due to cholesterol plaques that form on the inner lining. This is especially common at branching points of the leg arteries. The blockage of these arteries reduces blood flow to the leg muscles. When walking or exercising, the leg muscles require more blood flow to increase oxygen to the cells. Atherosclerotic plaques decrease blood flow and oxygen, causing the leg muscles to ache and burn. This is felt as cramping in the legs.
What are the symptoms of claudication?
Pain and cramping in the legs are the main symptoms of claudication. The pain can be sharp or dull, aching or throbbing, or burning. The severity of the peripheral artery disease, the location of the plaque, and the activity of the muscles determine the symptoms and the location of the pain. Calf pain is the most common location for leg cramps because the plaques often begin in the arteries farthest from the heart. If the blockage or plaque formation is farther up the leg, the pain from claudication may be felt in the thigh. If the blockage is in the aorta (the main artery from the heart to the legs), symptoms may include pain in the buttocks or groin or erectile dysfunction.
What can cause the artery narrowing that leads to claudication?
Intermittent claudication can be due to temporary artery narrowing due to vasospasm, permanent artery narrowing due to atherosclerosis, or complete blockage of a leg artery.
Why does claudication come and go?
The usually intermittent nature of claudication pain is due to a temporary inadequate supply of oxygen to the leg muscles. The poor oxygen supply is a result of narrowing of the leg arteries. This limits the oxygen supply and is especially noticeable when the muscles require more oxygen with exercise or walking. Claudication that comes and goes is often referred to as intermittent claudication.
Who gets claudication?
Intermittent claudication is more common in men than women. It affects 1% to 2% of the population under 60 years of age, increasing with age to affect over 18% of individuals over 70 years of age, according to the American Academy of Family Physicians.
How is claudication diagnosed?
A physician will take a history and diagnose based on the patient’s symptoms.
Testing for claudication may include:
- Ultrasound is commonly used to determine the location and severity of the narrowing in the blood vessels.
- Ankle-arm index measures the blood pressure at the ankle compared with the blood pressure in the arm. An abnormal result indicates peripheral artery disease.
- Segmental blood pressure measures blood pressure in different parts of the leg (calf, low thigh, high thigh) to detect a blockage causing decreased blood flow.
- Computed tomography (CT) and magnetic resonance angiography (MRA) are noninvasive tests that can help map the blood flow in the affected areas. These tests may be considered if a doctor thinks a procedure (revascularization) to treat peripheral artery disease may be helpful.
What is the treatment for claudication?
There are two main ways to treat claudication: medication and surgical revascularization.
Medication therapies are often used initially as they are non-invasive. The two most commonly used medications include:
- Cilostazol (Pletal) reduces the pain of intermittent claudication by dilating the arteries, improving blood and oxygen flow to the legs.
- Pentoxifylline (Trental) decreases blood viscosity, improving blood and oxygen flow through arteries to the muscles.
Several drugs are being investigated to treat claudication, with current approval. These medications include:
- ACE (angiotensin-converting enzyme) inhibitors
- Antichlamydophila therapy – roxithromycin
- Propionyl-L-carnitine
- Defibrotide
- Prostaglandins
A surgical procedure called revascularization is used in patients unresponsive to medications. There are two types of revascularization procedures: endovascular (inside the blood vessel) and surgical grafting or bypassing of the artery.
- Endovascular procedures include:
- Angioplasty: A balloon is placed in the blocked area and inflated to widen the artery and increase blood flow.
- Stenting: Wire mesh used to hold a blood vessel open after angioplasty, preventing scar tissue from narrowing the blood vessel.
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and understand that I may opt out of MedicineNet subscriptions at any time.
Can claudication be prevented?
Some risk factors for claudication can be modified, such as quitting smoking, managing diabetes and high blood pressure, and maintaining a healthy diet to keep cholesterol levels normal.
Medications that help thin the blood can be used to prevent claudication symptoms, but they do not treat the underlying cause. Medications include aspirin, clopidogrel (Plavix), ticlopidine (Ticlid), and dipyridamole (Permole, Persantine, Aggrenox).
Exercise is recommended for patients with claudication symptoms. Frequent exercise, especially walking, greatly reduces symptoms and increases symptom-free walking distance, making it one of the most effective preventive measures.
What is the prognosis and treatment for patients with intermittent claudication?
The prognosis of claudication is generally favorable with treatment. Without treatment, 26% of patients worsen over time. Over 5 years, 4% to 8% will progress to require a revascularization procedure.
The underlying cause of claudication, peripheral vascular disease, puts patients at risk for other atherosclerotic diseases. Finding claudication or peripheral artery disease should be considered a warning sign of other potential atherosclerotic blockages in the body.
Dominguez, JA, MD, et al. Peripheral Arterial Occlusive Disease. Medscape.
https://www.medscape.com/viewarticle/406951
Carman, T. L. and B. B. Fernandez. "A Primary Care Approach to the Patient with Claudication." American Family Physician.


