Contents
Actinic Keratosis
Actinic keratosis (AK), also known as solar keratosis, is a small, rough spot occurring on sun-exposed skin. These superficial spots are skin cancers that have not invaded the deeper layers of the skin. Actinic keratoses typically appear on photo-damaged skin.
Specialized forms of actinic keratoses include cutaneous horns, where the skin protrudes in a thick, hornlike manner, and actinic cheilitis, characterized by scaling and roughness of the lower lip and blurring of the border of the lip and adjacent skin. Cutaneous horns can also be caused by warts and age spots (seborrheic keratoses).
Causes of Actinic Keratoses
AK develops on the skin due to chronic sun exposure and is most common in fair-skinned individuals who have spent years outdoors or exposed their skin to indoor tanning radiation. Sun exposure can cause the skin to become wrinkled, mottled, and thinned.
Risk Factors for Actinic Keratoses
People at risk for AK include fair-skinned individuals who have spent years outdoors or exposed their skin to indoor tanning radiation. Other high-risk groups include organ transplant patients and those treated with PUVA therapy for psoriasis.
Symptoms and Signs
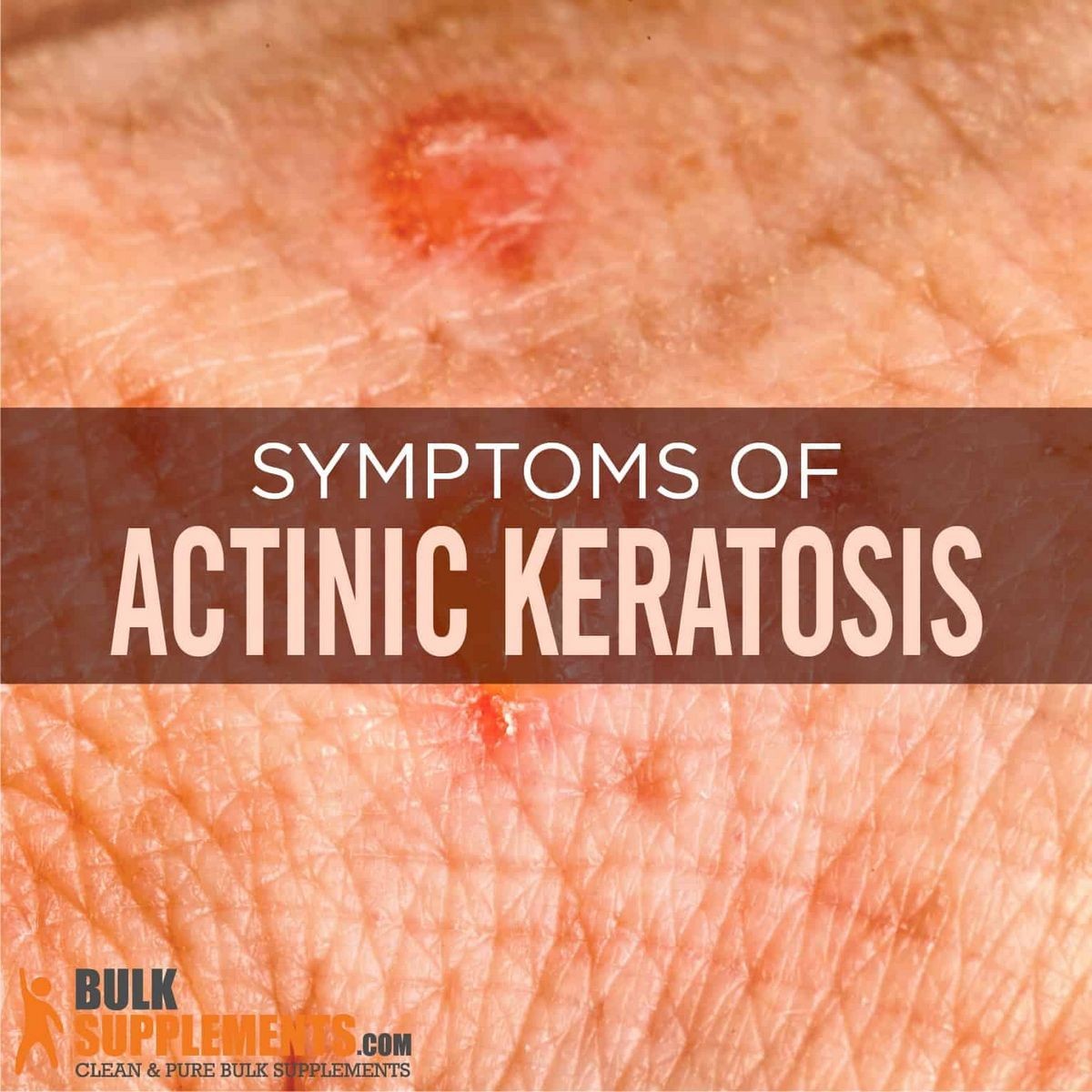
Actinic keratoses are usually between 2-6 mm in diameter, reddish in color with a rough texture, and often have a white or yellowish scale on top. They may cause a prickling pain when touched.
Locations
Common locations for actinic keratoses include the cheeks, bridge of the nose, rim of the ears, scalp, back of the neck, upper chest, tops of the hands, and forearms. Men are more likely to develop AKs on top of the ears or a bald pate, while long hair can provide some protection.
Significance of Actinic Keratosis
Actinic keratoses have the potential to develop into invasive skin cancer, although the chance of progression is less than 1%. However, individuals with many AKs who continue to expose their skin to ultraviolet sunlight are at higher risk. Treating actinic keratoses early can prevent invasive skin cancer.
Patients often express surprise when diagnosed with AK because they believe they have never been exposed to the sun. However, there can be a long delay for these keratoses to develop, and short periods of sun exposure do not usually cause or transform them into skin cancer.
IMAGES
Diagnosis of Actinic Keratoses
Primary care physicians or dermatologists can diagnose and care for actinic keratosis. In certain cases, a biopsy may be advisable to rule out skin cancer, especially if the lesion is large or thick. Seborrheic keratoses, raised brown lesions unrelated to sun exposure, may also require medical attention.
Treatment Options
The best treatment for AK is prevention. Minimizing sun exposure is crucial, although this may have limited effect once actinic keratoses develop. Treatment methods include cryosurgery (freezing with liquid nitrogen), other forms of surgery (scraping or burning off AKs), laser resurfacing, 5-fluorouracil (5-FU) creams, imiquimod (Aldara), ingenol mebutate (Picato), photodynamic therapy (PDT), diclofenac (Solaraze), and superficial chemical peels using trichloracetic acid (TCA).
Home Remedies
There are no home remedies for actinic keratoses, but many may resolve spontaneously if sun exposure is strictly limited. Lesions that do not resolve require professional medical attention.
Prognosis and Prevention
Patients with actinic keratoses should undergo yearly examination to prevent and detect invasive skin cancer. Avoiding excessive sun exposure decreases the risk of recurrences. Sun avoidance, including the use of sunscreens and protective clothing, is the simplest way to prevent actinic keratoses. Taking niacinamide and multivitamin supplements may also have some preventative benefits.
References:
Conforti, Claudio, Emanuela Beninanti, and Caterina Dianzani. "Are Actinic Keratoses Really Squamous Cell Cancer? How Do We Know if They Would Become Malignant?" Clinics in Dermatology (2017). doi: 10.1016/j.clindermatol.2017.08.01.
Costa, Claudia, et al. "How to Treat Actinic Keratosis? An Update." J Dermatol Case Rep 9.2 (2015): 29-35.
Uhlenhake, E.E. "Optimal treatment of actinic keratoses." Clin Interv Aging 8 (2013): 29-35.
Uhlenhake, E.E. "Optimal treatment of actinic keratoses." Clin Interv Aging 8 (2013): 29-35.


