Contents
Side Effects of Ery-Tab (erythromycin)
Ery-Tab (erythromycin) is a macrolide antibiotic used to treat streptococcal infections of the throat and skin; lung infections, such as pneumonia caused by Streptococcal pneumoniae, Mycoplasma pneumoniae, and Legionella pneumophila (Legionnaire’s disease); pelvic inflammatory disease (PID); erythrasma; whooping cough; listeriosis; and intestinal amebiasis.
Ery-Tab is also used to treat staphylococcal infections of the skin and as an alternative antibiotic for the treatment of syphilis, gonorrhea, and chlamydia.
Ery-Tab is used in patients who are allergic to penicillin for the prevention of recurrent rheumatic fever and infections of the hearts’ valves (endocarditis) in patients with valvular abnormalities of the heart before they undergo dental treatments.
The non-FDA approved uses for Ery-Tab include acne, Lyme disease, and tetanus. Ery-Tab prevents bacterial cells from growing and multiplying by interfering with their ability to make proteins while not affecting human cells. Bacteria such as Haemophilus influenzae are resistant to erythromycin alone and must be treated with a combination of erythromycin and adequate doses of sulfonamides.
Common side effects of Ery-Tab include:
Serious but rare side effects of Ery-Tab include allergic reactions such as:
- hives,
- rash, or
- anaphylaxis (a severe allergic reaction which can lead to shock and death).
Drug interactions of Ery-Tab include antiarrhythmic drugs, theophyllines, ergotamine or dihydroergotamine, digoxin, warfarin, HMG-CoA reductase inhibitors (statins), some anti-seizure drugs, sildenafil, and grapefruit juice.
Ery-Tab crosses the placenta, but its level in the blood of the fetus is low. There are no adequate studies in pregnant women, hence pregnant women should only use Ery-Tab if it is felt that the benefits of treatment outweigh the potential but unknown risks.
Ery-Tab is excreted in breast milk; however, Ery-Tab is considered by the American Academy of Pediatrics to be compatible with breastfeeding. Caution should be exercised, however, when Ery-Tab is prescribed to women who are breastfeeding.
What are the important side effects of Ery-Tab (erythromycin)?
The most frequent side effects of erythromycin are:
These gastrointestinal side effects are usually dose-related, i.e., more pronounced with higher doses.
Allergic reactions such as:
- hives,
- rash, or
- anaphylaxis (a severe allergic reaction which can lead to shock and death) have been reported rarely.
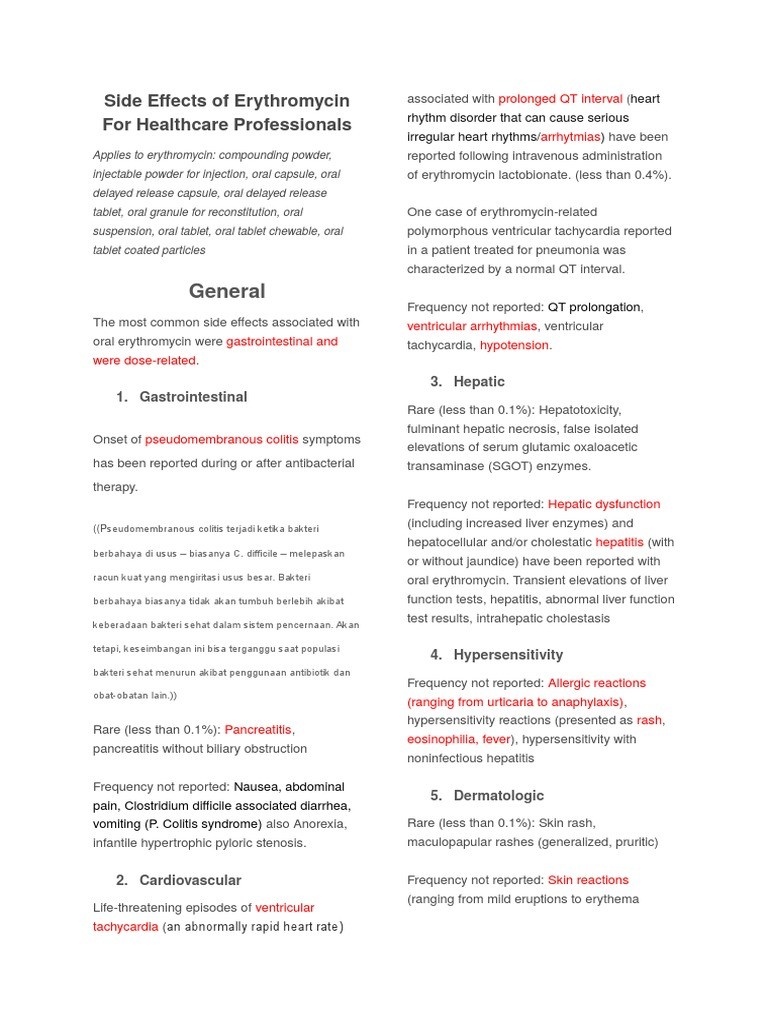
Ery-Tab (erythromycin) side effects list for healthcare professionals
The most frequent side effects of oral erythromycin preparations are gastrointestinal and are dose-related. They include:
Symptoms of hepatitis, hepatic dysfunction and/or abnormal liver function test results may occur.
Onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment.
Erythromycin has been associated with QT prolongation and ventricular arrhythmias, including ventricular tachycardia and torsades de pointes.
Allergic reactions ranging from urticaria to anaphylaxis have occurred. Skin reactions ranging from mild eruptions to erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis have been reported rarely.
There have been rare reports of pancreatitis and convulsions.
There have been isolated reports of reversible hearing loss occurring chiefly in patients with renal insufficiency and in patients receiving high doses of erythromycin.
What drugs interact with Ery-Tab (erythromycin)?
- Erythromycin use in patients who are receiving high doses of theophylline may be associated with an increase in serum theophylline levels and potential theophylline toxicity. In case of theophylline toxicity and/or elevated serum theophylline levels, the dose of theophylline should be reduced while the patient is receiving concomitant erythromycin therapy.
- Concomitant administration of erythromycin and digoxin has been reported to result in elevated digoxin serum levels.
- There have been reports of increased anticoagulant effects when erythromycin and oral anticoagulants were used concomitantly. Increased anticoagulation effects due to interactions of erythromycin with oral anticoagulants may be more pronounced in the elderly.
- Erythromycin is a substrate and inhibitor of the 3A isoform subfamily of the cytochrome p450 enzyme system (CYP3A). Coadministration of erythromycin and a drug primarily metabolized by CYP3A may be associated with elevations in drug concentrations that could increase or prolong both the therapeutic and adverse effects of the concomitant drug. Dosage adjustments may be considered, and when possible, serum concentrations of drugs primarily metabolized by CYP3A should be monitored closely in patients concurrently receiving erythromycin.
- The following are examples of some clinically significant CYP3A based drug interactions. Interactions with other drugs metabolized by the CYP3A isoform are also possible. The following CYP3A based drug interactions have been observed with erythromycin products in post-marketing experience:
- Ergotamine/dihydroergotamine: Concurrent use of erythromycin and ergotamine or dihydroergotamine has been associated in some patients with acute ergot toxicity characterized by severe peripheral vasospasm and dysesthesia.
- Triazolobenzodiazepines(such as triazolam and alprazolam) and related benzodiazepines: Erythromycin has been reported to decrease the clearance of triazolam and midazolam, and thus, may increase the pharmacologic effect of these benzodiazepines.
- HMG-CoA Reductase Inhibitors: Erythromycin has been reported to increase concentrations of HMG-CoA reductase inhibitors (e.g., lovastatin and simvastatin). Rare reports of rhabdomyolysis have been reported in patients taking these drugs concomitantly.
- Sildenafil (Viagra): Erythromycin has been reported to increase the systemic exposure (AUC) of sildenafil. Reduction of sildenafil dosage should be considered. (See Viagra package insert.)
- There have been spontaneous or published reports of CYP3A based interactions of erythromycin with cyclosporine, carbamazepine, tacrolimus, alfentanil, disopyramide, rifabutin, quinidine, methylprednisolone, cilostazol, vinblastine, and bromocriptine.
- Concomitant administration of erythromycin with cisapride, pimozide, astemizole, or terfenadine is contraindicated.
- In addition, there have been reports of interactions of erythromycin with drugs not thought to be metabolized by CYP3A, including hexobarbital, phenytoin, and valproate.
- Erythromycin has been reported to significantly alter the metabolism of the nonsedating antihistamines terfenadine and astemizole when taken concomitantly. Rare cases of serious cardiovascular adverse events, including electrocardiographic QT/QTc interval prolongation, cardiac arrest, torsades de pointes, and other ventricular arrhythmias have been observed. In addition, deaths have been reported rarely with concomitant administration of terfenadine and erythromycin.
- There have been post-marketing reports of drug interactions when erythromycin was coadministered with cisapride, resulting in QT prolongation, cardiac arrhythmias, ventricular tachycardia, ventricular fibrillation, and torsades de pointes most likely due to the inhibition of hepatic metabolism of cisapride by erythromycin. Fatalities have been reported.
- Drug/Laboratory Test interactions: Erythromycin interferes with the fluorometric determination of urinary catecholamines.
Summary
Ery-Tab (erythromycin) is a macrolide antibiotic used to treat various infections. Common side effects include gastrointestinal symptoms. There are no adequate studies in pregnant women. Ery-Tab is considered compatible with breastfeeding by the American Academy of Pediatrics.


