Contents
ACE Inhibitors vs. Beta Blockers
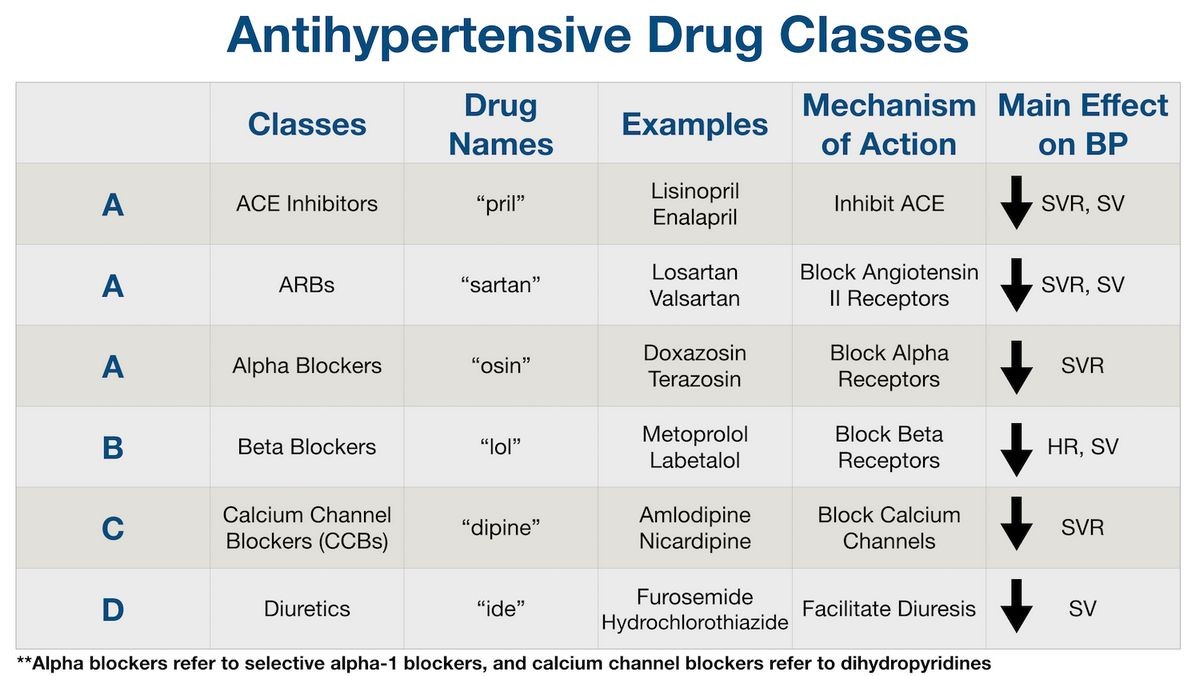
ACE inhibitors work by preventing angiotensin I from converting into angiotensin II, which narrows blood vessels. This helps relax blood vessels and lower blood pressure.
Beta-blockers block norepinephrine and epinephrine from binding to beta receptors on nerves. This helps reduce heart rate and lower blood pressure.
Side effects of ACE inhibitors and beta-blockers
ACE Inhibitor side effects
ACE inhibitors have side effects, and pregnant women and individuals with bilateral renal artery stenosis or severe reactions to ACE inhibitors should avoid them.
The most common side effects include cough, elevated blood potassium levels, low blood pressure, dizziness, headache, drowsiness, weakness, abnormal taste, rash, chest pain, increased uric acid levels, sun sensitivity, and increased BUN and creatinine levels.
The most serious side effects are kidney failure, allergic reactions, pancreatitis, liver dysfunction, a decrease in white blood cells, and swelling of tissues.
Beta blocker side effects
Beta-blockers slow heart rate and reduce blood pressure, but they may cause adverse effects such as heart failure or heart block in patients with heart problems.
Other side effects include headache, depression, confusion, dizziness, nightmares, hallucinations, shortness of breath in asthmatics, sexual dysfunction, and low or high blood glucose levels.
Other serious side effects include toxic epidermal necrolysis, Raynaud’s phenomenon, lupus erythematosus, bronchospasm, serious allergic reactions, erythema multiforme, Steven Johnson Syndrome, and toxic epidermal necrolysis.
Drug interactions with ACE inhibitors and beta-blockers
ACE Inhibitor drug interactions
ACE inhibitors have few interactions with other drugs.
However, ACE inhibitors may increase blood levels of potassium and the blood concentration of lithium, and reduce the blood pressure lowering effects of aspirin and other nonsteroidal anti-inflammatory drugs. They should also not be combined with ARBs, aliskiren, or injectable gold sodium aurothiomalate.
Beta-blocker drug interactions
Combining certain beta-blockers with thioridazine or chlorpromazine may result in low blood pressure and abnormal heart rhythms.
Combining clonidine with a beta-blocker or discontinuing their concurrent use may cause dangerous elevations in blood pressure. Phenobarbital and similar agents may reduce the effectiveness of beta-blockers, and aspirin and other NSAIDs may counteract the blood pressure reducing effects. Beta-blockers may also prolong hypoglycemia in diabetics.
Different types of ACE inhibitors and beta blockers
ACE inhibitors list
The following is a list of ACE inhibitors available in the United States:
- benazepril (Lotensin)
- captopril (Capoten- discontinued brand)
- enalapril (Vasotec, Epaned, [Lexxel- discontinued brand])
- fosinopril (Monopril- Discontinued brand)
- lisinopril (Prinivil, Zestril, Qbrelis)
- moexipril (Univasc- Discontinued brand)
- perindopril (Aceon)
- quinapril (Accupril)
- ramipril (Altace)
- trandolapril (Mavik)
Beta blockers list
The following is a list of beta-blockers available in the United States:
- acebutolol (Sectral)
- atenolol (Tenormin)
- betaxolol (Kerlone, Betoptic S)
- bisoprolol fumarate (Zebeta)
- carteolol (Cartrol, discontinued)
- carvedilol (Coreg)
- esmolol (Brevibloc)
- labetalol (Trandate [Normodyne – discontinued])
- metoprolol (Lopressor, Toprol XL)
- nadolol (Corgard)
- nebivolol (Bystolic)
- penbutolol (Levatol)
- pindolol (Visken, discontinued)
- propranolol (Hemangeol, Inderal LA, Inderal XL, InnoPran XL)
- sotalol (Betapace, Sorine)
- timolol (Blocadren, discontinued)
- timolol ophthalmic solution (Timoptic, Betimol, Istalol)
Summary
ACE inhibitors and beta-blockers are used to treat high blood pressure, congestive heart failure, prevent kidney failure, and reduce the risk of stroke. Learn more about their side effects and drug interactions.


