Contents
- 1 Why Would A Child Need A Tracheostomy?
- 1.0.1 Why would a child need a tracheostomy?
- 1.0.2 What are the difficulties in pediatric tracheostomy?
- 1.0.3 How is a pediatric tracheostomy performed?
- 1.0.4 How long does a child need a tracheostomy?
- 1.0.5 How do you care for a child with a tracheostomy?
- 1.0.6 What are the complications of a tracheostomy?
Why Would A Child Need A Tracheostomy?
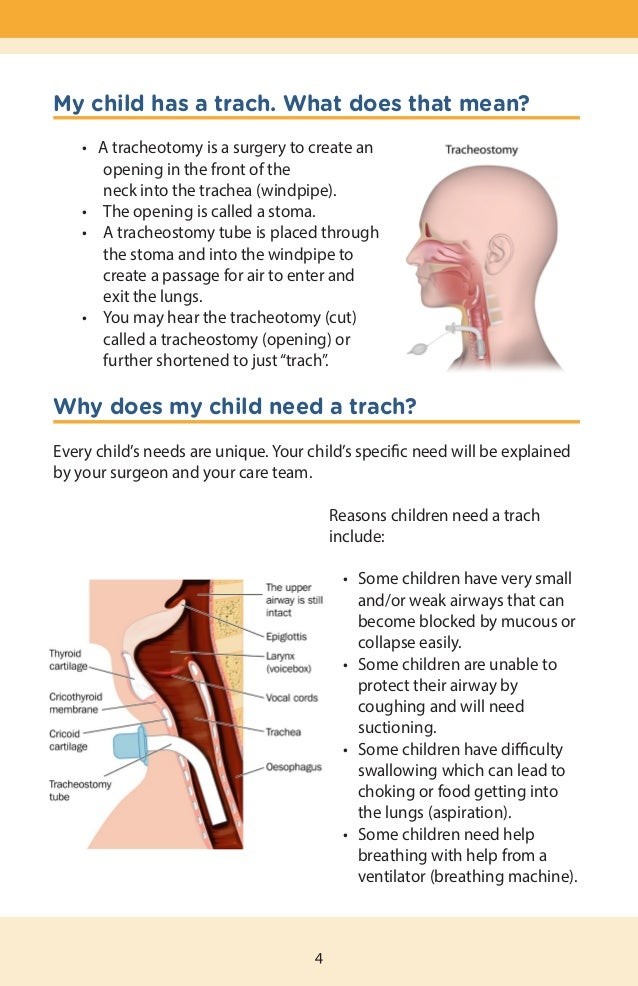
A tracheostomy is performed on children who have difficulty breathing or are unable to breathe on their own. It involves creating a small opening in the airway to insert a tube that provides assisted ventilation to the lungs.
A pediatric tracheostomy is a surgical procedure that creates an opening in the airway, below the vocal cords, in children. This allows a tube to be inserted into the trachea, enabling air to flow into the lungs when the upper airway is blocked or assisting with ventilation for children who cannot breathe on their own.
Why would a child need a tracheostomy?
A child may require a tracheostomy if they are unable to breathe without assistance. The most common reason for pediatric tracheostomy is prolonged reliance on assisted ventilation due to respiratory or neuromuscular disorders.
Tracheostomy was initially developed to treat children with upper airway blockage caused by infectious diseases like diphtheria and poliomyelitis. Vaccinations have now eradicated these diseases in most parts of the world.
Nowadays, pediatric tracheostomy is mainly performed in the following situations:
- Anticipated long-term lung and/or heart function insufficiency
- Presence of upper airway obstruction that will likely persist for an extended period
Some conditions that may require a pediatric tracheostomy include:
- Subglottic stenosis (narrowing of the airway below the vocal cords)
- Bilateral vocal cord paralysis
- Congenital airway malformations
- Respiratory papillomatosis (benign or malignant airway tumors)
- Ingestion of corrosive substances
- Craniofacial syndromes (skull or facial malformation)
What are the difficulties in pediatric tracheostomy?
Pediatric tracheostomy is more challenging than in adults due to the delicate and underdeveloped tissues of children. The following anatomical characteristics of a child’s neck can complicate the procedure:
- The lung’s membrane (pleura) extends into the neck, increasing the risk of lung injury.
- The pliable trachea can be difficult to identify by palpation.
- The trachea may be deep in the throat, requiring careful differentiation from the carotid blood vessels.
- The short length of the neck allows for less working space.
- Inadequate identification of the cricoid cartilage around the larynx can lead to injury.
>
How is a pediatric tracheostomy performed?
A pediatric surgeon performs a tracheostomy on a child under general anesthesia. The procedure typically takes around 45 minutes.
Preparation
- The surgeon selects a tracheostomy tube of appropriate size based on the child’s age and weight.
- The child must stop eating and drinking a few hours before the procedure (in elective cases).
- If the child has a nasogastric feeding tube, it is removed.
- The pediatric anesthesiologist administers general anesthesia and places an endotracheal tube through the mouth, unless the child is already intubated for assisted ventilation.
- The child lies on their back with a roll under the shoulders to extend the neck.
Procedure
The surgeon typically follows these steps:
- Administers local anesthesia in the throat area.
- Makes a horizontal incision in the skin, midway between the cricoid cartilage and the top of the sternum (sternal notch).
- Retracts the skin and cuts and cauterizes the fat and muscle layers to prevent bleeding and infection.
- Cuts or retracts the thyroid isthmus, which connects the right and left lobes of the thyroid gland, to expose the trachea.
- Places nonabsorbable stay sutures on both sides of the trachea’s midline.
- Elevates and exposes the trachea on the skin surface.
- Makes a vertical incision in the middle of the trachea.
- Sutures the skin flaps to the trachea.
- Simultaneously removes the endotracheal tube and inserts the tracheostomy tube.
- Connects the ventilator to the tracheostomy tube and ensures its proper functioning.
- Tapes the stay sutures on the chest and applies gauze dressing to the tracheostomy site.
Post-procedure
Imaging tests are conducted to evaluate the tube’s position and lung condition, particularly for possible pneumothorax (collapsed lung). The child remains in intensive care for about a week to allow the stoma to heal and the first tube to be replaced.
The tracheostomy tube is removed (decannulation) once the child can breathe independently through the upper airway and no longer requires assisted ventilation. If decannulation is challenging, a bronchoscopy or microlaryngoscopy may be performed to check for airway obstruction and larynx mobility.
The tube is temporarily plugged to assess the child’s ability to breathe without support. Upon tube removal, the opening is taped shut, and the wound typically closes within a week. In some cases, a surgical closure may be necessary.
How long does a child need a tracheostomy?
Most tracheostomies are temporary and used until the underlying condition is resolved. Premature babies may require a tracheostomy tube for several weeks based on their gestational age.
Tracheostomy may be permanent for children with permanent upper airway or larynx damage or loss of function. The tube size will be adjusted as the child grows.
How do you care for a child with a tracheostomy?
If a child requires a tracheostomy for an extended period, they can be cared for at home. Before starting home care, the family or caregiver must undergo a structured training program at the hospital. Essential components of home care for a child with a tracheostomy include:
- Cleaning and changing the tube
- Suctioning secretions to keep the tube clear
- Humidifying the inhaled air
- Applying medications
- Maintaining cleanliness and sterility of the stoma and tube
- Dressing and protecting the stoma
What are the complications of a tracheostomy?
Complications of a tracheostomy can include:
Early complications
- Pneumomediastinum (air leak into the space between the lungs)
- Pneumothorax
- Subcutaneous emphysema (trapped air under the skin)
- Acute hemorrhage
- Accidental tube dislodgement
- Tube obstruction
Intermediate complications
- Infection at the stoma leading to excessive tissue growth (granulation), making tube removal or replacement difficult
Late complications
- Difficulty in decannulation due to stoma granulation
- Tracheal obstruction from granulation
- Accidental decannulation as the child gains mobility
- Subglottic stenosis
- Tracheal stenosis
- Suprastomal collapse (collapse of the trachea above the stoma)
- Tracheocutaneous fistula (abnormal channel between the trachea and subcutaneous tissue)
- Speech and language development issues
Source: Operative Techniques in Otolaryngology, 2020, Elsevier


