Contents
What Does a Rheumatoid Arthritis Rash Look Like?
People with rheumatoid arthritis (RA) must prioritize their health and care for their skin.
Rheumatoid arthritis (RA) is an autoimmune disease that causes joint swelling and inflammation, which can also affect the skin. Skin problems can occur in people with severe RA and in the early stages of RA.
Symptoms of a rheumatoid arthritis rash
Common symptoms of rheumatoid arthritis (RA) rash include:
- Red patches
- Burgundy patches on darker skin tones; may appear as pinpoint dots
- Swelling
- Itchiness
- Develops on fingertips, toes, and elbows; can occur anywhere on the body
- Rarely, deep red pinpricks may appear
- Advanced cases may develop ulcers or lesions
- Rash site may have thin, wrinkly skin prone to bruises
- Rash may cause pale, translucent, and dry skin
- Redness on palms and back of hands
- Nail changes
Although rare, these rashes can cause painful ulcers that can become infected and complicate treatment and healing.
Known skin complications in people with rheumatoid arthritis
RA symptoms vary in severity, including possible skin complications.
These severe skin conditions can manifest in people with RA:
- Rheumatoid vasculitis – Swollen blood vessels causing symptoms ranging from red, itchy rashes to skin ulcers; mainly seen on the legs.
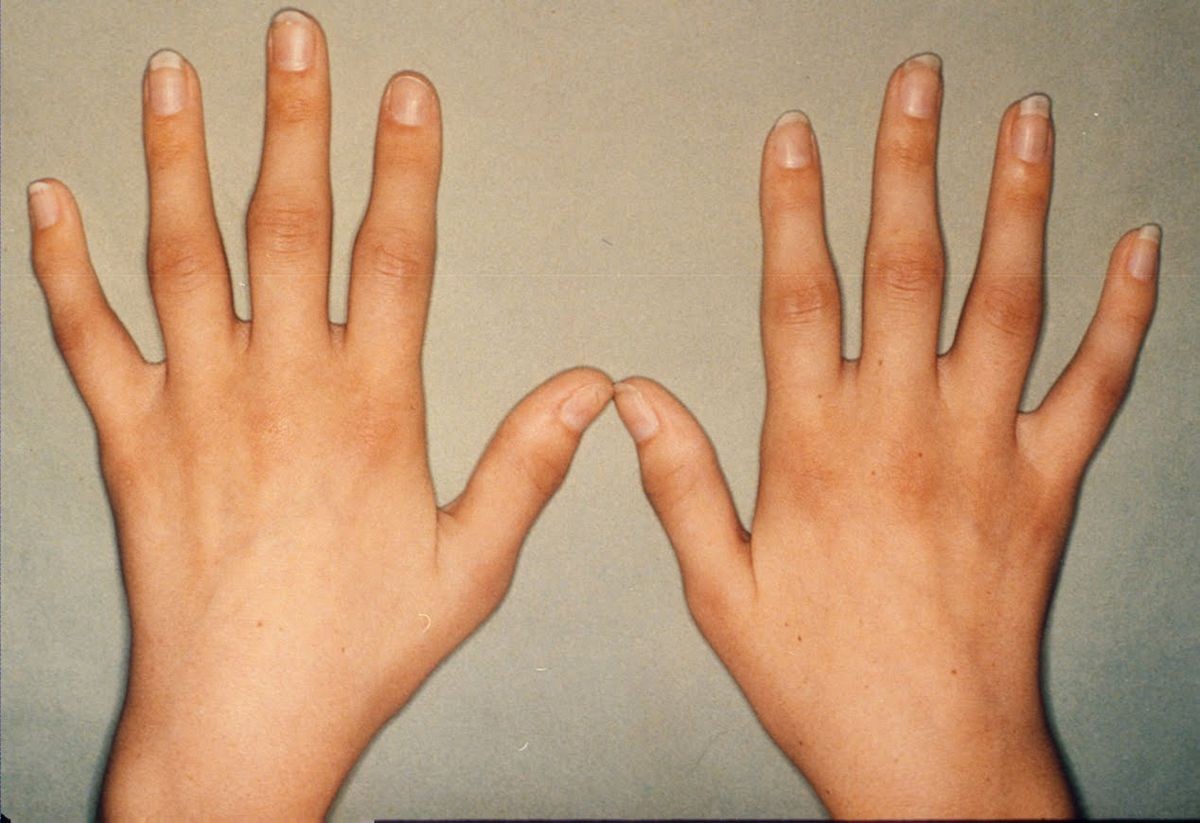
- Reddened palms, also known as palmar erythema – Common and affects both hands, causing warmth.
- Livedo reticularis – Mottled patches resembling eczema; rare and can change in size and shape.
- Dermatomyositis – Purple, lace-like rash on the legs; harmless but should be treated if associated with another medical condition.
- Urticaria (hives) – Red, itchy welts; increasingly recognized as a symptom of RA.
- Neutrophilic dermatosis (NLD) – Raised rash on arms and legs; first sign is typically on a single limb or torso.
- Raynaud’s phenomenon – Constricted blood vessels causing color changes, discomfort, and delayed healing.
- Rheumatoid nodules – Tissue lumps that form under the skin, usually over bony areas.
- Atopic dermatitis – Eczema-like rash; studies show link between atopic dermatitis and RA.
- Sweet’s syndrome – Painful, blistering rash with mucosal lesions.
- Pyoderma gangrenosum – Ulcerative rash with bluish borders, fresh ulcers, and minimal skin damage; serious condition requiring medical attention.
Treatment options for a rheumatoid arthritis rash
A comprehensive treatment plan combines nonpharmacologic interventions, pharmaceutical modalities, and surgery. Inflammation control is crucial for symptom management and disease progression prevention. Consult a rheumatologist to determine the best treatment course based on your symptoms.
Nonpharmacologic measures
- Rest
- Nutritious diet
- Occupational therapy
- Exercises
- Paraffin baths
Pharmacologic therapy
- Disease-modifying antirheumatic drugs (DMARDs) – Prescribed for RA to halt disease progression and should be administered within three months of diagnosis.
- Biologic response modifiers – Additional treatment when DMARDs don’t provide desired response; target specific immune cells to reduce inflammation.
- Janus kinase (JAK) inhibitors – Reduce immune responses damaging joints; bear risks of infections and illnesses due to weakened immune system.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – Offer supplementary therapy and pain relief in conjunction with corticosteroids or as needed; opioid painkillers prescribed for severe pain and carefully managed due to addiction risk.
- Corticosteroids – Adjunctive therapy for inflammation and discomfort; prolonged use discouraged.
- Antibiotics – Topical, oral, or both if infection risk exists.
There are no permanent solutions to prevent RA rashes entirely. Your doctor may prescribe a combination of medications to manage your condition, reduce inflammation, and prevent joint damage. It’s crucial for people with RA to prioritize their health and skincare.


