Contents
Trigeminal Neuralgia
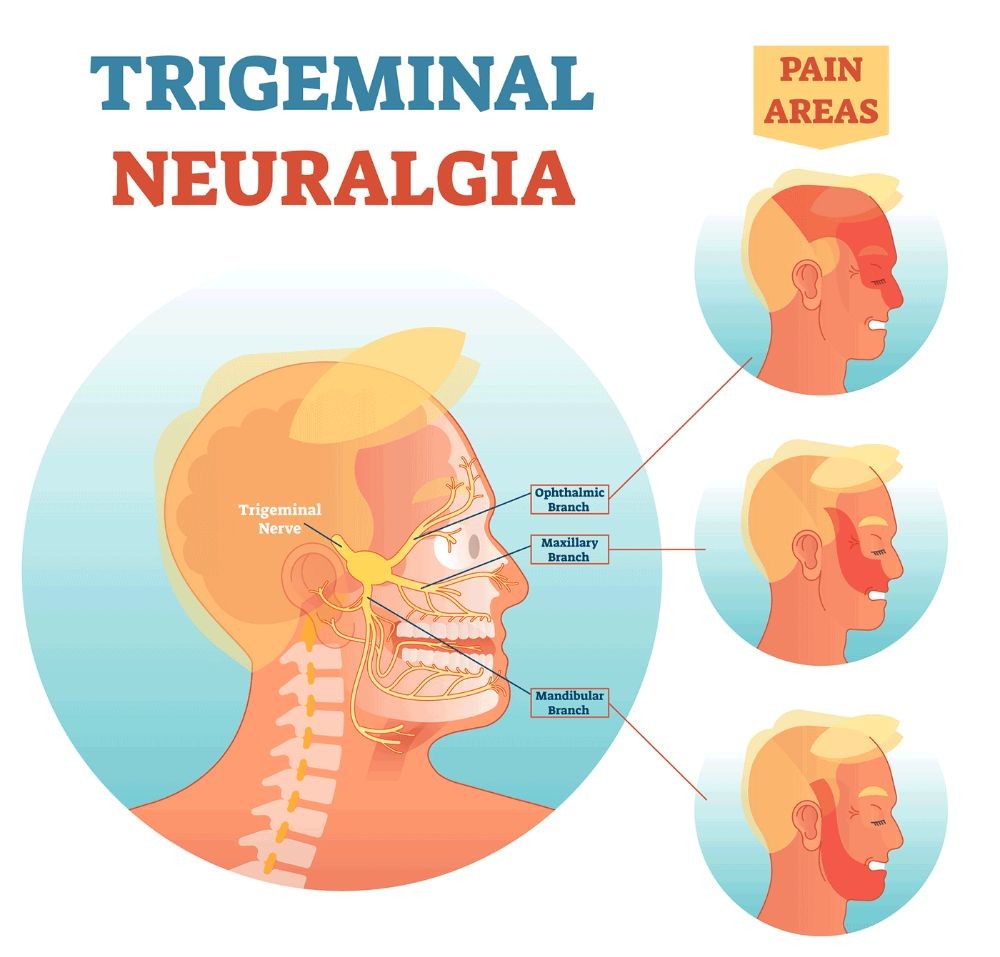
Trigeminal neuralgia is inflammation of the trigeminal nerve, causing intense facial pain. It is also known as tic douloureax because the pain can cause patients to contort their face and move their head. This movement is known as a tic.
The pain of trigeminal neuralgia is intense and may be an isolated episode or occur every few hours, minutes, or seconds. There can be months or years between attacks, but in some patients, it can lead to chronic pain syndrome, affecting daily life and causing depression.
Though it can affect people of any age, trigeminal neuralgia tends to afflict people older than 60 years. It affects the right side of the face five times more often than the left.
Women are affected more often than men. People with multiple sclerosis are affected more frequently than the general population.
12 Cranial Nerves and their function
The brain is connected to the body by the spinal cord with spinal nerves sending and receiving impulses and messages to and from the brain. However, there are twelve cranial nerves that directly connect to the body. These nerves are involved with the muscle and sensory function of the head and neck. (The exception is cranial nerve X or the vagus nerve, which is also responsible for the parasympathetic system of the chest and abdomen).
| Olvactory | Smell |
| Optic | Vision |
| Oculomotor, Trochlear, Abducens | Eye movement |
| Trigeminal | Facial sensation, chewing |
| Facial | Facial movement |
| Auditory | Hearing |
| Glossopharyngeal | Taste, swallowing |
| Vagus | Swallowing, voice modulation, parasympathetic tone of the body |
| Accessory | Neck muscles |
| Hypoglossal | Swallowing, speech articulation |
The trigeminal nerve (cranial nerve V) is so named because it has three branches responsible for face sensation; one branch also regulates chewing.
- The ophthalmic branch (V1) is responsible for sensation from the scalp, forehead, upper eyelid, and tip of the nose.
- The maxillary branch (V2) sensation covers the lower eyelid, the side of the nose, the upper lip and cheek, and the upper teeth and gums.
- The mandibular branch (V3) is responsible for the sensation of the lower teeth and gums, lower lip, chin, jaw, and part of the ear. It is also responsible for supplying the muscles involved with chewing.
What causes trigeminal neuralgia?
Most often, the cause of trigeminal neuralgia is unknown.
- There are instances when the nerve can be compressed by nearby blood vessels, aneurysms, or tumors.
- There are inflammatory causes of trigeminal neuralgia due to systemic diseases including multiple sclerosis, sarcoidosis, and Lyme disease.
- There is also an association with collagen vascular diseases including scleroderma and systemic lupus erythematosus.
What are the symptoms of trigeminal neuralgia?
Symptoms of trigeminal neuralgia include sharp, stabbing pain on one side of the face. It tends to begin at the angle of the jaw and radiate along the junction lines between the ophthalmic branchV1 and maxillary branch V2, or the maxillary branch V2 and the mandibular branch V3.
- The pain is severe and described as an electric shock. It may be made worse by light touch, chewing, or cold exposure in the mouth. In the midst of an attack, affected individuals shield their faces to protect them. This is an important diagnostic sign because, with many other pain syndromes like toothache, the person will rub or hold the face to ease the pain.
- While there may be only one attack of pain, the person may experience recurrent sharp pain every few hours or seconds. Between the attacks, the pain resolves completely and the person has no symptoms. However, because of fear that the intense pain might return, people can be quite distraught.
- Trigeminal neuralgia tends not to occur when the person is asleep, differentiating it from migraines, which often wake the person.
- After the first episode of attacks, the pain may subside for months or years but there is always the risk that trigeminal neuralgia will recur without warning.
How is trigeminal neuralgia diagnosed?
Idiopathic trigeminal neuralgia is a clinical diagnosis and often no testing is required after the healthcare professional takes a history and performs a physical examination which should be normal.
It is important to note that the neurologic exam must be normal. There can be no muscle weakness; V3 is responsible for chewing and there can be no jaw or facial weakness found. The corneal reflex controlled by V1 must be present. When the cornea is touched, the eye blinks in response. If these two findings are not normal, the search should begin for an inflammatory or compression cause of the trigeminal nerve. Some clinicians may order an MRI to help diagnose other conditions that may cause trigeminal neuralgia.
The International Headache Society has established 5 criteria for making the diagnosis:
- Paroxysmal attacks of pain lasting from a fraction of a second to 2 minutes, affecting 1 or more divisions of the trigeminal nerve and fulfilling criteria B and C.
- Pain has at least one of the following characteristics: (1) intense, sharp, superficial, or stabbing; or (2) precipitated from trigger areas or by trigger factors
- Attacks stereotyped in the individual patient
- No clinically evident neurologic deficit
- Not attributed to another disorder
What is the treatment for trigeminal neuralgia?
- Idiopathic trigeminal neuralgia is often treated with a single anticonvulsant medication such as carbamazepine (Tegretol).
- Gabapentin (Neurontin, Gabarone), baclofen, and phenytoin (Dilantin, Dilantin-125) may be used as second-line drugs, often in addition to carbamazepine. In many patients, as time progresses, carbamazepine becomes less effective and these drugs can be used in combination to control the pain.
- Lamotrigine (Lamictal) may be prescribed for multiple sclerosis patients who develop trigeminal neuralgia.
- If pain persists and medication fails to be effective, surgery or radiation therapy may be other treatment options.
- There are no effective home remedies for trigeminal neuralgia.
- Eat mushy foods or liquidize meals if you’re having difficulty chewing.
- Certain foods seem to trigger attacks in some people, so you may want to consider avoiding things such as caffeine, citrus fruits, and bananas.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
Medically reviewed by Joseph Carcione, DO; American Board of Psychiatry and Neurology
The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24 Suppl 1:9-160.