Contents
How Long Can You Live With Niemann–Pick Disease?
Niemann–Pick disease (NP) leads to a gradual loss of function of nerves, the brain, and other organs.
NP is a rare but fatal condition in infancy. The life expectancy for NP varies depending on the type. Prognosis is strongly related to the age at which the neurological manifestations appear and is generally poor, with affected individuals expected to live only 10 to 20 years after diagnosis.
NP is a group of inherited metabolic disorders known as lipid storage diseases. The disease is classified into:
- Type A: Child rarely survives beyond 18 months. Some live to age four.
- Type B: Children may survive until late childhood or early adulthood, but their quality of life is poor. They may need supplemental oxygen due to lung impairment.
- Types C and D: Always fatal, but the prognosis depends on the time of diagnosis. The child is likely to live into their late teens or early twenties. Some die as children, while others can live into adulthood.
People with NP have varying life expectancies. A child who exhibits NP symptoms before age one may not survive to school age. People who develop symptoms after starting school may live into their late teens, with a few surviving into their twenties.
What are the signs and symptoms of Niemann–Pick disease?
NP can damage the brain, nerves, liver, spleen, bone marrow, and, in severe instances, the lungs. People with this disorder have symptoms due to the gradual loss of function of nerves, the brain, and other organs.
Type A
Infantile or acute form of NP. Symptoms may progress rapidly and include:
- Hepatosplenomegaly (enlargement of the liver and spleen)
- Musculoskeletal abnormalities
- Degenerative muscle weakness and floppiness
- Seizures and muscular spasms
- Macula (Pigmentation in the tissue of the eyes may occur. Cherry-red spots may be seen.)
- Jaundice
- Fever
- Gastrointestinal problems, such as vomiting, diarrhea, and abdominal distention
- Swollen lymph nodes
- Difficulty feeding
- Difficulty performing basic motor skills
- Poor muscle tone
- Brain damage along with neurological problems (loss of reflexes)
- Lung disease and frequent respiratory infections
Type B
The chronic form of NP. Symptoms progress slowly and begin during infancy or early childhood. These include:
- No or minimal neurological involvement
- Hepatosplenomegaly (abnormal enlargement of the liver and spleen)
- Macula (the formation of cherry-red spots on the eyes)
- Slow growth rate
- Increased incidence of respiratory infections
- Respiratory infections
- Low blood platelets
- Poor coordination
- Mental retardation
- Psychiatric disorders
- Peripheral nerve problems
- Lung problems
- High lipids in the blood
- Short stature
Type C
It includes two subtypes: NPC1 and NPC2. The progression of symptoms in NP type C is slow, and the loss of mental and motor function usually occurs in early adulthood. Symptoms include:
- Hepatosplenomegaly (the liver and spleen may be moderately enlarged)
- Musculoskeletal dysfunctions
- Psychomotor dysfunction
- Seizures
- Tremors
- Spasticity of the muscles
- Extreme muscle weakness
- Ataxia (inability to coordinate voluntary muscle movements)
- Vertical gaze palsy (results in difficulty or loss of up and down movement)
- Ophthalmoplegia (loss of muscle ability to move eyes)
- Dysarthria (inability to form and speak words clearly)
- Jaundice
- Difficulty learning
- Decline in intellect
- Difficulty speaking and swallowing
- Clumsiness
- Loss of vision or hearing
- Brain damage
Type D
The symptoms of type D are very similar to those of type C but may vary from case to case.
Type E
Many researchers consider this a variant of type C. Symptoms usually do not begin until adulthood, and neurological impairment is rare. Symptoms include:
- Hepatosplenomegaly
- Dementia (progressive and irreversible)
- Confusion
- Disorientation
- Deterioration of intellectual capacity and function and impaired memory
- Ataxia
- Ophthalmoplegia
Type F or sea-blue histocyte disease or mild form of type B
It is characterized by:
- Sea-blue-colored cells in the blood and/or bone marrow
- Hepatosplenomegaly
- Cirrhosis (thickened tissue obstructing blood flow through the liver)
- Mild thrombocytopenia (decrease in platelet count)
- Macula (pigmentation in the tissue of the eyes, with a white ring around the maculae)
- Absence of hair in the armpit area
Type A is the most severe form and manifests in early childhood. Type B is most common during adolescence. Type C can appear in childhood or develop in adolescence or adulthood. Research on other types is limited.
What causes Niemann–Pick disease?
NP is a type of lipid storage disease that is inherited. In NP, lipids (fatty materials) and proteins are not broken down, leading to toxic lipids building up in various cells and causing a progressive deterioration of the nervous system.
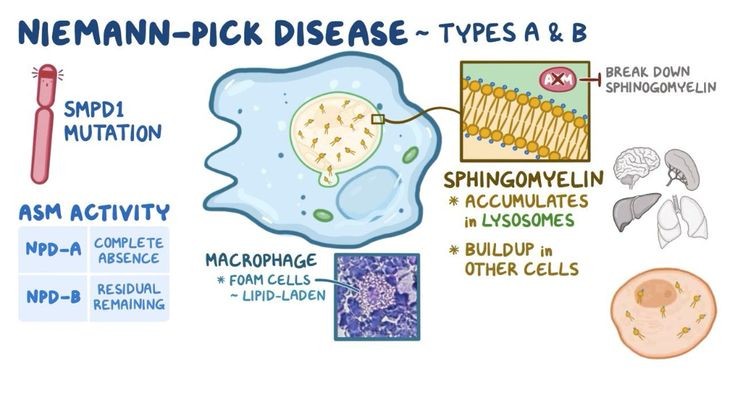
NP occurs due to mutations in specific genes responsible for lipid metabolism.
- Types A and B: Caused when WBCs inhibit the production of sphingomyelinase, which leads to fat accumulation in cells.
- Type C: Occurs due to an inability to get rid of lipids or cholesterol.
- Other types: Causes may be similar to types A, B, and C, with some having unknown causes.
- Inheritance: NP is a genetic disorder, and both parents must have the faulty gene for their child to get the disease.
Risk factors
- Family members with NP
- Ashkenazi Jewish heritage (types A and B)
- North African ancestry, Maghreb region (type B)
- Spanish–American population of southern New Mexico and Colorado (type C)
- Nova Scotia, French–Canadian ancestry (type D)
- Type F affects people of Spanish descent, while the affected populations of type E are unclear.
Scientists are investigating how lipid accumulation in these diseases causes harm to the body. Additional research is being conducted to identify biomarkers, indications, other causes, and risk factors.
What are the treatment options for people with Niemann–Pick disease?
NP is incurable, but treatment aims to alleviate symptoms and improve quality of life.
A doctor may recommend the following treatments:
- Nutrition: Monitoring calorie intake and planning a diet to provide necessary nutrients for growth and development. In some cases, a feeding tube may be necessary.
- Medication: Sedatives for sleep and irritability, statins to lower cholesterol, antidepressants, CNS stimulants, anticonvulsant drugs, anticholinergic drugs, botulinum toxin, and laxatives for gastrointestinal issues.
- Therapy: Physical and occupational therapy to encourage movement and prevent contracture, and multidisciplinary treatment for behavioral problems.
- Transfusion: Blood transfusion for decreased platelet count.
- Bone marrow transplant: Beneficial for certain types of NP to improve enzyme function, red blood cell count, and liver size.
- Pain management: Analgesics.
- Monitoring and supportive treatment: Monitoring blood lipid levels and liver functions.
- Oxygen therapy: Keeping the person stable.
- Emerging treatments: Drugs like miglustat, transplantation of organs, enzyme replacement and gene therapies, lipid-lowering drug combinations, cyclodextrin, stem cell transplantation, and combination treatments.
If you have a family history of NP and plan to have children, genetic counseling and screening are advised.
If you have a family history of NP and plan to have children, genetic counseling and screening are advised.


