Contents
- 1 Does Prurigo Nodularis Ever Go Away?
- 1.0.1 What is prurigo nodularis?
- 1.0.2 What does prurigo nodularis (PN) look like?
- 1.0.3 What triggers prurigo nodularis?
- 1.0.4 How do you test for prurigo nodularis?
- 1.0.5 How do I get rid of prurigo nodularis?
- 1.0.6 Is prurigo nodularis serious?
- 1.0.7 Subscribe to MedicineNet’s Skin Care & Conditions Newsletter
Does Prurigo Nodularis Ever Go Away?
Prurigo nodularis (PN), also called nodular prurigo, is difficult to treat because success depends on how well the person adheres to the treatment.
PN is a chronic condition that can last for years. Itchy bumps or nodules on the skin can be relieved by breaking the itch-scratch cycle, but they rarely heal without proper medications and lifestyle changes. While therapy can reduce symptoms’ intensity, they tend to persist over time.
However, treatments may improve patients’ quality of life.
What is prurigo nodularis?
Prurigo nodularis (PN) is a rare skin condition with no known cause, although it appears to be an autoimmune disease. Some believe that it arises due to immune dysregulation in the skin.
PN leads to the development of cutaneous nodules that cause extreme skin irritation. Itchy bumps can create a cycle of itching and scratching, leading to more nodules and inflamed skin. Constant scratching prevents nodules from healing, resulting in scarring. The itching can be severe enough to cause bleeding or discomfort.
What does prurigo nodularis (PN) look like?
Signs and symptoms of prurigo nodularis (PN) include:
- Hard, irritating nodules on the skin of the arms, legs, stomach, neck, back, and other areas.
- Nodules usually don’t develop on the face, palms, or soles of the feet.
- Multiple nodular skin lesions can appear as tiny red lumps. They can cause constant or intermittent episodes of acute itching.
- Nodules can range in size from a few millimeters to over 3 centimeters.
- Crusting and scaling can occur on scratched lesions.
- Repetitive scratching can cause permanent skin changes like thickening and dark pigmentation.
- The skin between the nodules is typically dry and itchy. New nodules may form, but old ones may fade and leave scars.
- Secondary infections, stress, and depression can occur.
PN can cause severe itching, especially at night or when the nodules touch clothes. Itching often resolves only after scratching to the point of bleeding or discomfort, which can lead to infections.
IMAGES
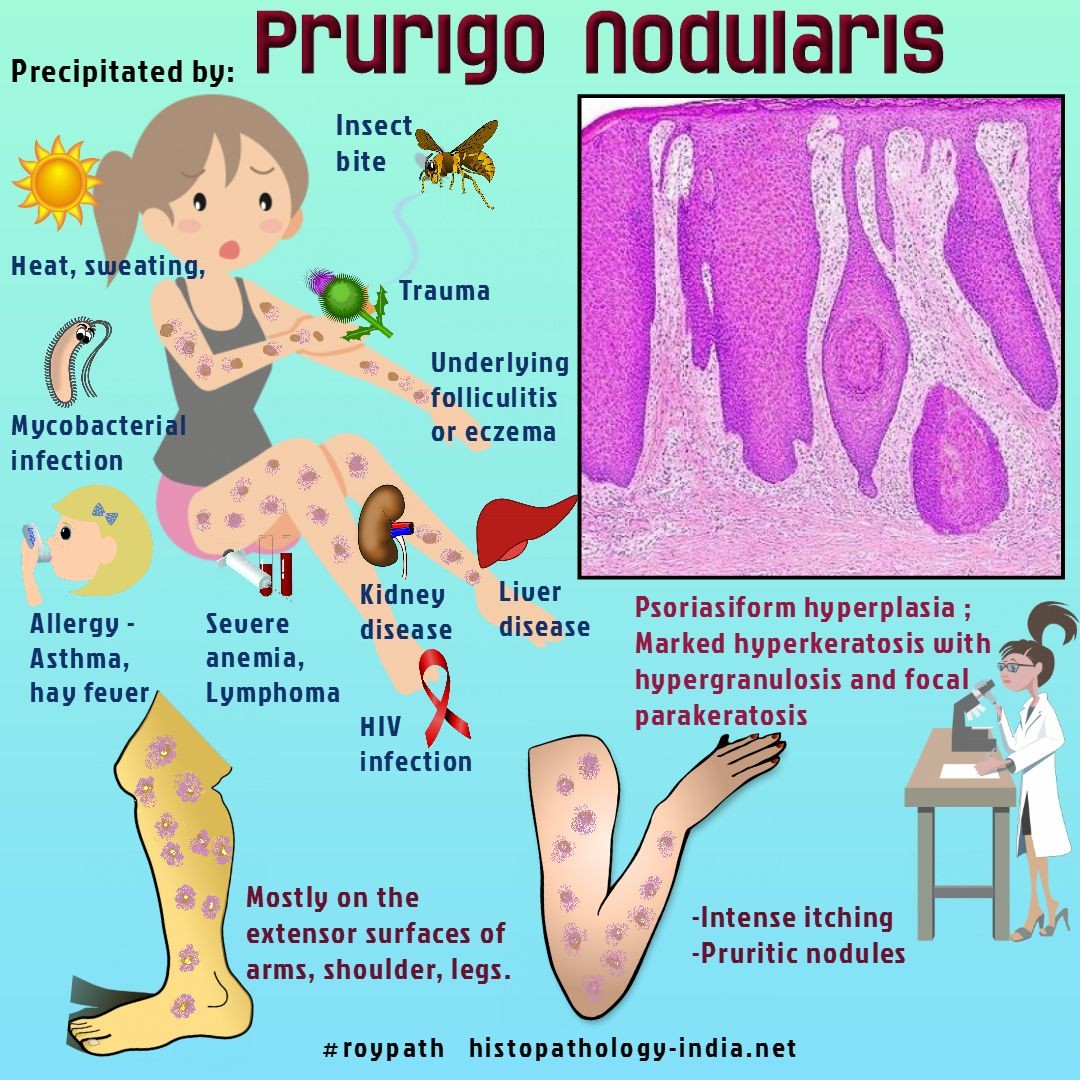
What triggers prurigo nodularis?
The specific cause of prurigo nodularis (PN) is unknown, but symptoms are likely due to nerve and immune system abnormalities in the skin. PN can be found in patients with stasis eczematous dermatitis.
PN can develop at any age but is most common in individuals between 20 and 60. Both sexes are affected equally.
Possible risk factors for PN include:
- Race: African Americans are at higher risk.
- Genetics: Autoimmunity and genetics are involved in its progression. In 50% of cases, an inherited condition like asthma, eczema, hay fever, or hives is present.
- Personal or family history: Many patients have a history of eczema, atopic dermatitis, asthma, hay fever, or other allergies.
- Insect bites: PN may be triggered by insect bites and underlying infections.
- Underlying conditions: PN is associated with various diseases and conditions such as kidney failure, HIV, hepatitis C, thyroid disease, lymphoma, liver disease, iron deficiency anemia, and more.
- Strict diets: PN is frequently referred to as a "keto rash" because it is associated with patients who follow strict diets like the ketogenic diet.
- Gut imbalance: Imbalance in the gut microbiota may be implicated in PN, affecting the immune system.
- Medications: PN can be caused by certain drugs, such as chemotherapeutic drugs.
- Others: Sweating, clothing, heat, and emotional stress can exacerbate symptoms.
PN is fairly common, especially in patients with related or precipitating conditions, but its general population prevalence has not been studied. Patients with PN typically have underlying causes related to atopy, psychology, and nutrition.
How do you test for prurigo nodularis?
Diagnosis is typically made based on clinical signs and treatment response. Dermatologists may suspect prurigo nodularis (PN) when a patient has severely itchy skin and nodules.
To confirm a diagnosis of PN, a skin biopsy may be performed. Under a microscope, the skin will appear swollen and abnormal, sometimes mimicking squamous cell carcinoma. Nerve fibers and terminals may also be enlarged.
Your dermatologist may recommend blood tests and other investigations to understand the possible underlying causes of PN.
How do I get rid of prurigo nodularis?
The goal of prurigo nodularis (PN) treatment is to resolve or minimize itching and prevent skin pigmentation. By breaking the itch-scratch cycle, the nodules and damaged skin can recover.
The most popular methods of treating PN involve using topical or intralesional steroids. Phototherapy or systemic immunosuppressives may be necessary in severe cases or when treatment resistance occurs.
Localized treatment
- Emollients (sometimes with methanol)
- Steroids (topical, intralesional, or intravenous)
- Phenol and local anesthetic lotions
- Coal tar creams
- Calcipotriol ointment
- Capsaicin cream
- Cryotherapy with liquid nitrogen
- Pulsed dye laser (reduces vascularity of lesions)
Systemic treatment
- Antihistamines
- Corticosteroids (systemic)
- Immunosuppressives (cyclosporin, methotrexate, azathioprine)
- Thalidomide (in severe cases)
- Naltrexone (opiate-receptor antagonist)
- Systemic retinoids (acitretin)
- UV exposure
- Psoralen combined with ultraviolet A treatment
- Immunomodulatory roxithromycin with or without tranilast
- Gabapentin
Breaking the itch-scratch cycle
- Psychological counseling
- Habit reversal therapy
- Anxiolytic drugs
- Antidepressants (amitriptyline, doxepin)
Self-care and trigger prevention
- Avoid using soaps or shower gels that dry out the skin.
- Apply emollients regularly to maintain good skin health.
- Monitor side effects and undergo regular blood tests.
- Control the urge to scratch.
- Keep fingernails trimmed.
- Keep rooms cool and avoid heavy bedding while sleeping.
- Wear breathable clothing.
- Wear gloves or mittens while sleeping to avoid scratching.
Dietary modifications
Maintain a balanced diet while limiting refined foods and increasing anti-inflammatory foods.
- Foods to avoid: Trans fat, red meat, fried food, processed food with high levels of additives and preservatives, refined sugar and flour.
- Foods to include: Starchy vegetables, fruits, legumes, whole grains, spices, wholesome fats, dark chocolate, green tea.
Investigational therapies
- Thalidomide
- Lenalidomide
- Opioid receptor antagonists
- Neurokinin-1 receptor antagonists
- Monoclonal antibody therapies
Is prurigo nodularis serious?
Prurigo nodularis (PN) can take time to properly manage. Patients may benefit from a combination of topical treatments, medications, and lifestyle adjustments.
PN is an inflammatory skin condition with underlying comorbidities. Studies have reported a link between PN and cancer. PN is classified as a disability because of its rarity and severity.
PN can be difficult to treat and may not fully resolve. It is important to follow your dermatologist’s advice and report any problems with your therapy.
Subscribe to MedicineNet’s Skin Care & Conditions Newsletter
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and understand that I may opt out of subscriptions at any time.
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and understand that I may opt out of subscriptions at any time.