Contents
Anthrax (Bacillus Anthracis)
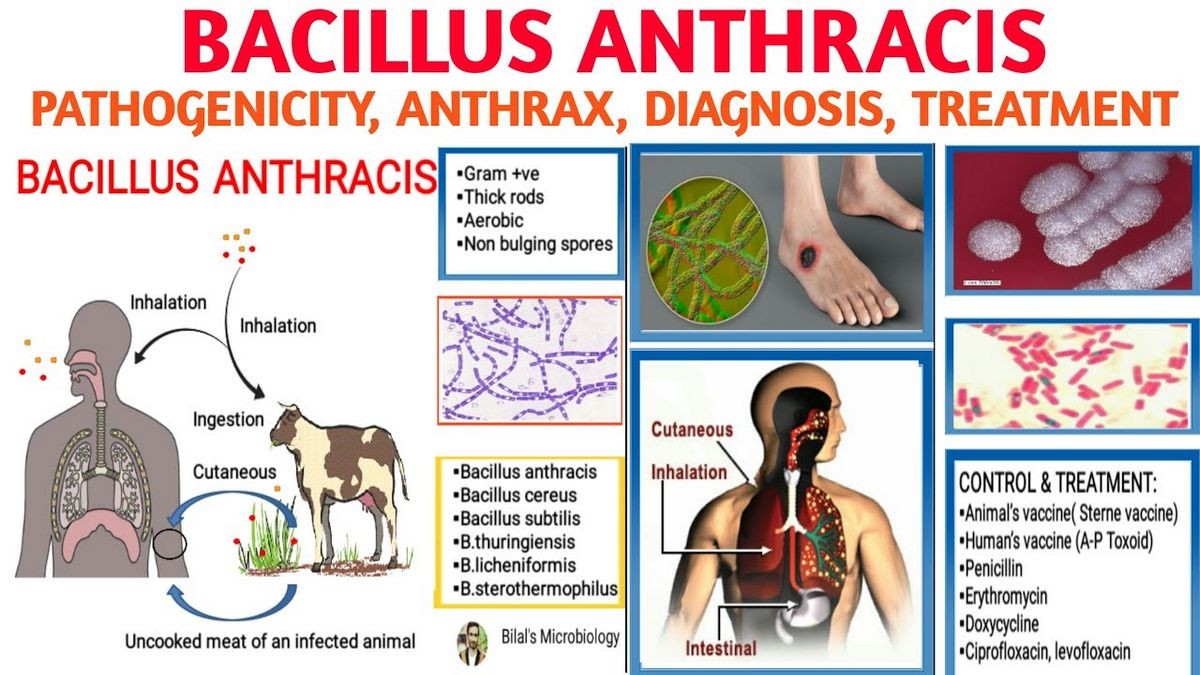
Anthrax is a life-threatening infectious disease caused by Bacillus anthracis that primarily affects animals, especially ruminants (goats, cattle, sheep, and horses). Anthrax can be transmitted to humans through contact with infected animals or their products. Recently, anthrax has gained attention as it can also be spread through bioterrorist attacks or biological warfare. Anthrax does not spread from person to person and is not contagious.
There have been localized outbreaks of anthrax over the years. In Siberia, Russia in 2016, a major outbreak occurred, resulting in sickness among at least 13 Siberian individuals and the death of over 2,000 reindeer. This outbreak was believed to have been caused by the melting permafrost unearthing a reindeer carcass infected with anthrax, which had been buried for 75 years, leading to the release of anthrax spores.
The causative agent of anthrax is Bacillus anthracis, a bacterium. Anthrax organisms exist in a dormant form called spores in the soil, where they are hardy and difficult to destroy. These spores can survive for up to 48 years. The bacteria secrete toxins composed of three proteins: protective antigen, lethal factor, and edema factor.
What causes anthrax?
Anthrax is now rare in humans in the United States and developed countries. It still occurs in countries with inadequate public-health regulations that prevent exposure to infected animals and their products. In recent years, there have been rare cases of anthrax in individuals exposed to imported animal hides used for making drums. Those at higher risk of infection include veterinarians, livestock producers and farmers, travelers to endemic areas, handlers of animal products, laboratory personnel studying anthrax, and individuals trained to respond to bioterrorists or biological warfare.
- Veterinarians
- Livestock producers and farmers
- Travelers to endemic areas
- Handlers of animal products
- Laboratory personnel studying anthrax
- Mail handlers, military personnel, and individuals trained to respond to bioterrorists/biological warfare
There are three ways in which anthrax can infect humans. The most common is infection through the skin, resulting in a dark sore. Anthrax can also be ingested from consuming contaminated meat, leading to serious, sometimes fatal disease. The most deadly form is inhalation anthrax, where spores inhaled they migrate to lymph glands in the chest, spread, and produce toxins that often cause death.
The incubation period for anthrax varies, but symptoms typically appear within one to five days. However, it can take weeks before an infected individual feels unwell.
What are the symptoms of anthrax?
Anthrax causes four forms of the disease: cutaneous, inhalation, gastrointestinal, and injection anthrax.
Cutaneous anthrax
The cutaneous form (80% of all anthrax infections) starts as a red-brown raised spot that enlarges with considerable redness around it, blistering, and hardening. An ulcer crater with blood-tinged drainage and the formation of a black crust, called an eschar, develops in the center of the spot. Swollen lymph nodes are also present. Other symptoms include muscle aches, pain, headache, fever, nausea, and vomiting. The illness typically resolves in about six weeks with appropriate antibiotics.
Injection anthrax
This new form of anthrax has been identified in heroin-injecting drug users in northern Europe but has not yet been reported in the United States. Symptoms may take days to months to appear and include small blisters or bumps that may itch at the injection site, fever and chills, swelling around the sores, and development of deep abscesses under the skin or muscle. Painless skin sores with black centers (dark scabs) may appear after the blisters or bumps.
Inhalation anthrax
The first symptoms are subtle, resembling flu-like symptoms, such as a sore throat and headaches. The illness progresses rapidly, with severe respiratory distress, shortness of breath, chest and/or muscle pain, coughing up blood, and, in some cases, shock, coma, and death. Inhalation anthrax does not cause pneumonia but affects lymph glands in the chest, where spores multiply and produce toxins that spread throughout the body. Most affected individuals will die, even with appropriate antibiotics, as the antibiotics do not destroy the already released deadly toxins.
Gastrointestinal anthrax
Gastrointestinal anthrax, now rare, results from consuming undercooked, contaminated meat. Symptoms include nausea, loss of appetite, bloody diarrhea, fever, and abdominal pain. The bacteria invade the bowel wall and spread through the bloodstream, leading to septicemia and life-threatening toxicity.
Diagnosis of anthrax
Primary-care doctors and pediatricians can treat anthrax, but consulting an infectious-disease specialist is advised. Other specialists who may be involved in diagnosing and treating anthrax include emergency-medicine specialists, pulmonologists, critical-care specialists, and physicians specializing in treating biologic agents used in warfare. Diagnosis is based on the person’s history, which may include occupation and possible exposure. Cultures or smears may be taken in cutaneous anthrax cases, while throat swabs, sputum, and chest X-rays are used in pulmonary anthrax. In disseminated cases, bacteria can be seen in the blood. Unusual manifestations may occur in bioterrorism attacks, such as the 2001 anthrax attack in the U.S. through anthrax spores spread as a white powder through the postal system.
What is the treatment for anthrax?
Most cases of anthrax can be cured with early treatment. Cutaneous anthrax can be treated with common antibiotics like penicillin, tetracycline, erythromycin, and ciprofloxacin. The pulmonary form of anthrax is a medical emergency requiring intravenous antibiotics. In the case of bioterrorism attacks, individuals exposed to anthrax may be given antibiotics as a preventive measure. A vaccine exists but is not yet widely available. Postexposure prevention involves a combination of antibiotics and a three-dose series of the anthrax vaccine.
What is the prognosis for anthrax?
The prognosis for anthrax infections depends on the type of infection and the promptness of antibiotic treatment. Inhalation anthrax has the worst prognosis, while the other forms have a range of outcomes depending on timely diagnosis, severity of infection, and organ system involvement.
Is it possible to prevent anthrax?
Public-health measures are crucial in preventing contact with infected animals. A vaccine is available for individuals at high risk, and efforts are being made to prevent bioterrorist attacks and prepare for their consequences. Research and development are ongoing to create more effective and safer anthrax vaccines, including oral alternatives to injection.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.
By clicking Submit, I agree to the MedicineNet’s Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet’s subscriptions at any time.